Preparing for a Nurse Practitioner (NP) interview is a crucial step in advancing your healthcare career. This role is unique as it combines clinical expertise with a holistic approach to patient care, allowing NPs to diagnose, treat, and manage a variety of health conditions independently. Proper interview preparation is essential, as it not only boosts your confidence but also showcases your knowledge, skills, and passion for patient advocacy. In this comprehensive guide, we will cover key interview questions, effective preparation strategies, tips for demonstrating your clinical competency, and how to convey your commitment to patient-centered care, ensuring you present yourself as a standout candidate in a competitive field.
What to Expect in a Nurse Practitioner Interview
In a Nurse Practitioner interview, candidates can expect a structured format that may include both behavioral and clinical questions. Interviews are often conducted by a panel that may consist of physicians, fellow nurse practitioners, and administrative staff. The process usually begins with an introduction, followed by questions assessing clinical knowledge, patient management skills, and situational judgment. Candidates may also be asked to discuss their experience and approach to patient care. Additionally, role-playing scenarios or case studies might be used to evaluate decision-making and clinical reasoning abilities.
Nurse Practitioner Interview Questions For Freshers
This set of Nurse Practitioner interview questions is tailored for freshers entering the field. It covers essential concepts, including clinical skills, patient communication, and healthcare regulations that candidates should be familiar with to demonstrate their readiness for the role.
1. What is the role of a Nurse Practitioner?
A Nurse Practitioner (NP) is a registered nurse with advanced clinical training and education, allowing them to diagnose and manage various medical conditions. NPs can perform physical exams, interpret diagnostic tests, and initiate treatment plans. They play a vital role in healthcare by providing high-quality, patient-centered care in various settings, including clinics, hospitals, and community health organizations.
2. What are the educational requirements to become a Nurse Practitioner?
To become a Nurse Practitioner, one must first obtain a Bachelor of Science in Nursing (BSN) and then complete a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP) program. After completing the educational requirements, candidates must pass a national certification exam in their specialty area to practice as an NP.
3. Can you explain the different specialties within Nurse Practitioners?
- Pediatric Nurse Practitioners: Focus on the healthcare of infants, children, and adolescents.
- Family Nurse Practitioners: Provide comprehensive care to patients of all ages, emphasizing health promotion and disease prevention.
- Adult-Gerontology Nurse Practitioners: Specialize in treating adult patients, including the elderly population.
- Psychiatric-Mental Health Nurse Practitioners: Offer mental health services, including diagnosis and treatment of psychiatric disorders.
Each specialty has specific training and certification requirements tailored to the population served.
Build your resume in just 5 minutes with AI.
4. What is your approach to patient education?
My approach to patient education involves assessing the patient’s understanding and tailoring the information to suit their level of comprehension. I utilize teach-back methods to ensure they grasp the concepts discussed. Additionally, I provide written materials and resources to reinforce learning and encourage patients to ask questions, fostering an open dialogue about their health.
5. How do you handle difficult patients?
Handling difficult patients requires patience and effective communication. I remain calm and listen actively to their concerns, validating their feelings. Establishing rapport is crucial, so I try to understand their perspective and work collaboratively to find a solution. If necessary, I involve other healthcare team members to address the situation more effectively.
6. What is the significance of evidence-based practice in nursing?
Evidence-based practice (EBP) is essential in nursing as it integrates clinical expertise, patient values, and the best available research evidence to guide decision-making. EBP improves patient outcomes, enhances quality of care, and ensures that nursing interventions are scientifically validated. By applying EBP, Nurse Practitioners can provide the most effective and up-to-date care for their patients.
7. Describe your experience with electronic health records (EHR).
In my training, I have become proficient in using electronic health records (EHR) systems to document patient information, track treatment plans, and communicate with other healthcare providers. I understand the importance of maintaining accurate and secure patient records, as well as adhering to regulations such as HIPAA to protect patient confidentiality.
8. How do you prioritize patient care in a busy environment?
Prioritizing patient care in a busy environment involves assessing the urgency of each patient’s needs and effectively managing time. I utilize triage principles to identify critical cases that require immediate attention while ensuring that all patients receive timely care. Collaboration with the healthcare team is vital to delegate tasks and streamline workflows, ensuring optimal patient outcomes.
9. What is your understanding of the Nurse Practice Act?
The Nurse Practice Act is a set of laws that define the scope of nursing practice within a specific state. It outlines the legal limitations and responsibilities of nurse practitioners, ensuring that they operate within their licensed capacity. Understanding the Nurse Practice Act is crucial for compliance and safeguarding patient care, as it governs professional conduct and licensure requirements.
10. How do you stay current with medical guidelines and best practices?
I stay current with medical guidelines and best practices by regularly reading peer-reviewed journals, attending professional conferences, and participating in continuing education courses. Engaging with professional organizations and collaborating with colleagues also helps me remain informed about the latest developments in healthcare, ensuring that my practice is evidence-based and up to date.
11. What strategies do you use to manage time effectively during patient visits?
To manage time effectively during patient visits, I prepare by reviewing patient records beforehand and setting clear objectives for each appointment. I utilize structured templates for documentation to save time and ensure thoroughness. Additionally, I encourage patients to come prepared with questions, which helps streamline the visit and allows for a more focused discussion.
12. How do you assess a patient’s mental health?
Assessing a patient’s mental health involves conducting a comprehensive evaluation that includes a detailed history, standardized screening tools, and direct observation of behavior. I engage in open dialogue to understand their thoughts, feelings, and behaviors, while also considering any physical symptoms that may impact their mental health. Collaborating with mental health professionals is also essential for accurate diagnosis and treatment.
13. What role does cultural competence play in nursing?
Cultural competence is critical in nursing as it enables practitioners to provide care that respects the diverse backgrounds and beliefs of patients. Understanding cultural differences influences communication, treatment preferences, and health literacy. By being culturally competent, Nurse Practitioners can build trust with patients, improve care outcomes, and promote health equity in diverse populations.
14. Can you explain the importance of pharmacology in nursing practice?
Pharmacology is vital in nursing practice as it involves understanding medications, their effects, interactions, and potential side effects. Nurse Practitioners prescribe and manage medications, so a strong foundation in pharmacology ensures safe and effective treatment for patients. This knowledge is essential for educating patients about their medications and monitoring their responses to therapy.
15. How do you approach teamwork in a healthcare setting?
I value teamwork in a healthcare setting, as it enhances patient care and fosters collaboration among professionals. I promote open communication, respect diverse perspectives, and actively participate in team meetings. By building strong relationships with colleagues, I facilitate information sharing and coordinated care, ultimately leading to improved patient outcomes and a positive work environment.
Nurse Practitioner Intermediate Interview Questions
As Nurse Practitioners (NPs) advance in their careers, they encounter more complex clinical scenarios and patient management challenges. Intermediate-level interview questions often explore advanced assessment skills, treatment planning, and interdisciplinary collaboration. Candidates should be well-versed in clinical guidelines, pharmacology, and patient education.
16. What are the key components of a comprehensive patient assessment?
A comprehensive patient assessment includes several critical components: patient history, physical examination, diagnostic testing, and psychosocial evaluation. The history covers medical, family, and social aspects, while the physical exam assesses the patient’s current health status. Diagnostic tests are utilized to confirm or rule out conditions, and psychosocial evaluation addresses emotional and mental health concerns, ensuring a holistic approach to patient care.
17. How do you differentiate between a viral and bacterial infection?
- Symptoms: Viral infections often present with systemic symptoms like fever, fatigue, and body aches, while bacterial infections may show localized symptoms such as redness, swelling, and pus.
- Lab Tests: Rapid tests, cultures, and sensitivity tests can help identify bacterial infections. Elevated white blood cell counts and specific markers like CRP may indicate bacterial presence.
Understanding these differences is crucial for appropriate prescribing and management, as antibiotics are ineffective against viral infections.
18. Describe your approach to managing chronic pain in patients.
When managing chronic pain, I employ a multidisciplinary approach that includes thorough assessment, patient education, and individualized treatment plans. This may involve medication management, physical therapy, behavioral therapy, and alternative therapies like acupuncture. Regular follow-ups are essential to adjust treatment as needed and to provide ongoing support to the patient.
19. What are the considerations when prescribing medications to elderly patients?
- Polypharmacy: Older adults often take multiple medications, increasing the risk of drug interactions and side effects.
- Renal and Hepatic Function: Dosing adjustments may be necessary based on renal and liver function, which can decline with age.
- Adherence: Simplifying medication regimens and providing clear instructions can improve adherence.
It is vital to conduct a thorough medication review and consider non-pharmacological alternatives when appropriate.
20. Explain the role of patient education in managing chronic diseases.
Patient education is critical in managing chronic diseases as it empowers patients to take an active role in their health. It involves teaching patients about their condition, treatment options, lifestyle modifications, and self-monitoring techniques. Effective education can improve adherence, enhance self-management skills, and ultimately lead to better health outcomes and quality of life.
21. How do you handle difficult conversations with patients, such as discussing terminal diagnoses?
Handling difficult conversations requires empathy, active listening, and clear communication. I approach such discussions by creating a safe environment, ensuring privacy, and allowing the patient to express their feelings. I provide clear, honest information while being sensitive to the patient’s emotional state. It is essential to discuss options and support systems available, helping the patient feel supported throughout the process.
22. What strategies do you use to prevent burnout in your practice?
- Self-Care: Prioritizing physical and mental well-being through regular exercise, healthy eating, and adequate rest.
- Support Networks: Engaging in peer support and professional counseling when needed.
- Time Management: Effectively managing time and setting realistic goals for patient care.
By implementing these strategies, I can maintain my effectiveness and compassion in patient care while reducing the risk of burnout.
23. Discuss the importance of interdisciplinary collaboration in patient care.
Interdisciplinary collaboration enhances patient care by bringing together diverse expertise to address complex health issues. It allows for comprehensive treatment planning and coordination of care, ensuring that all aspects of a patient’s health are considered. This teamwork can lead to improved patient outcomes, enhanced communication among providers, and greater patient satisfaction.
24. How do you stay current with medical guidelines and practices?
- Continuous Education: I regularly attend workshops, conferences, and webinars focused on my specialty.
- Professional Journals: Subscribing to and reading peer-reviewed journals helps me stay informed on the latest research and clinical guidelines.
- Networking: Engaging with colleagues and participating in professional organizations allows for knowledge sharing and collaboration.
These practices ensure that I provide evidence-based care to my patients.
25. What are the key considerations when developing a treatment plan for a patient with multiple comorbidities?
- Prioritization: Identifying which conditions require immediate attention and which can be managed simultaneously.
- Medication Management: Carefully selecting medications to minimize interactions and side effects.
- Patient Preferences: Involving the patient in decision-making to ensure that treatment aligns with their values and lifestyle.
A comprehensive approach is essential to optimize health outcomes while addressing the complexities of comorbid conditions.
26. Describe your experience with telehealth and its impact on patient care.
Telehealth has significantly expanded access to care, particularly for patients in remote areas or with mobility issues. My experience includes conducting virtual consultations, managing follow-ups, and using telehealth platforms for chronic disease management. This approach allows for timely interventions and fosters patient engagement while ensuring continuity of care, especially during unprecedented times like the COVID-19 pandemic.
27. How do you evaluate the effectiveness of a treatment plan?
- Patient Feedback: Regularly obtaining feedback from patients about their symptoms and overall satisfaction with the treatment.
- Clinical Outcomes: Monitoring objective measures such as lab results, vital signs, and functional status to assess improvement.
- Follow-up Assessments: Scheduling periodic follow-ups to review progress and make necessary adjustments to the treatment plan.
Evaluating effectiveness is an ongoing process that ensures optimal patient care and outcomes.
28. What role does cultural competence play in nursing practice?
Cultural competence is vital in nursing practice as it enhances the ability to provide effective care to diverse populations. It involves understanding and respecting cultural differences, which can influence health beliefs and behaviors. Culturally competent care promotes trust, improves communication, and ultimately leads to better patient outcomes by ensuring that care is tailored to individual needs.
29. How do you approach end-of-life care discussions with patients and families?
End-of-life care discussions require sensitivity and compassion. I approach these conversations by creating a comfortable environment, allowing for open dialogue about fears, wishes, and concerns. I provide information about options for palliative care and hospice services, ensuring that patients and families feel supported in their decisions. Respecting their values and preferences is paramount in this process.
30. What are your strategies for managing time effectively during patient appointments?
- Prioritization: I focus on the most critical issues first and allocate time based on patient needs.
- Structured Visits: Using a consistent format for appointments helps streamline the process and reduces time spent on non-essential tasks.
- Technology: Leveraging electronic health records and other tools to access patient information quickly and document efficiently.
Effective time management ensures that I provide thorough care while respecting patients’ time.
Nurse Practitioner Interview Questions for Experienced
This section includes interview questions tailored for experienced Nurse Practitioners, focusing on advanced topics such as patient management, clinical decision-making, and leadership skills. These questions are designed to evaluate expertise and the ability to handle complex clinical scenarios effectively.
31. How do you approach developing a treatment plan for a complex patient case?
When developing a treatment plan for a complex patient case, I consider the patient’s comprehensive medical history, current medications, and presenting symptoms. I also involve interdisciplinary collaboration, ensuring input from specialists as needed. The plan includes specific goals, interventions, and follow-up strategies, and I always ensure that the patient understands and agrees with the plan to enhance adherence.
32. Can you describe a time when you had to mentor a junior nurse or NP? What approach did you take?
In my previous role, I mentored a new Nurse Practitioner who was struggling with patient assessments. I took a hands-on approach, providing shadowing opportunities and constructive feedback. I also set aside time for regular check-ins where we discussed her experiences and challenges. This collaborative effort helped boost her confidence and improved her clinical skills significantly.
33. What strategies do you use for optimizing patient flow in a busy clinic?
- Efficient Scheduling: I analyze patient needs and adjust appointment lengths, ensuring adequate time for complex cases while maintaining flow.
- Utilizing Technology: Implementing electronic health records and online scheduling to streamline processes and reduce administrative burdens.
- Team Coordination: Regular meetings with staff to assess bottlenecks and adjust workflow as necessary, promoting a collaborative environment.
These strategies help in minimizing wait times and enhancing patient satisfaction while ensuring that quality care is maintained.
34. How do you ensure compliance with healthcare regulations and standards in your practice?
I ensure compliance by staying current with healthcare laws and regulations through continuous education and attending relevant seminars. Regular audits of patient records and procedures help identify areas needing improvement. Additionally, I foster a culture of compliance within the team by conducting training sessions and encouraging open discussions about regulations and best practices.
35. Describe how you handle conflicts with colleagues in a clinical setting.
When conflicts arise, I prioritize open communication. I first seek to understand the colleague’s perspective and then share my viewpoint respectfully. If necessary, I involve a mediator to facilitate the discussion. My goal is to reach a resolution that benefits our patients and maintains a positive work environment, focusing on collaboration rather than confrontation.
36. What role does evidence-based practice play in your decision-making process?
Evidence-based practice is central to my decision-making process. I continuously review the latest research and guidelines to inform my clinical judgments. By integrating clinical expertise with the best available evidence, I can provide high-quality patient care that is both effective and aligned with current standards, ultimately improving patient outcomes.
37. How do you approach patient education, especially for those with chronic conditions?
- Individualized Education: I tailor education to meet the specific needs and understanding of each patient, ensuring relevance.
- Utilizing Resources: I provide written materials and recommend reputable online resources to reinforce concepts.
- Follow-Up: I schedule follow-up appointments to address any questions and assess the patient’s understanding and adherence to the management plan.
This comprehensive approach fosters patient engagement and empowers them to manage their conditions effectively.
38. Can you discuss your experience with telehealth and its impact on patient care?
My experience with telehealth has been positive, allowing for greater access to care, particularly for patients in rural areas. It facilitates timely consultations and follow-ups, improving patient engagement. I ensure that telehealth sessions are conducted securely and that I maintain the same level of professionalism and thoroughness as in-person visits to ensure quality care.
39. How do you assess the effectiveness of a treatment plan over time?
- Monitoring Outcomes: I track key health indicators and patient feedback to evaluate the effectiveness of the treatment.
- Regular Follow-ups: Scheduled follow-ups provide opportunities to adjust treatment based on the patient’s progress and any emerging issues.
- Patient Engagement: I encourage patients to share their experiences and any side effects, fostering a collaborative approach to their care.
This systematic assessment helps in refining the treatment plan to ensure optimal patient outcomes.
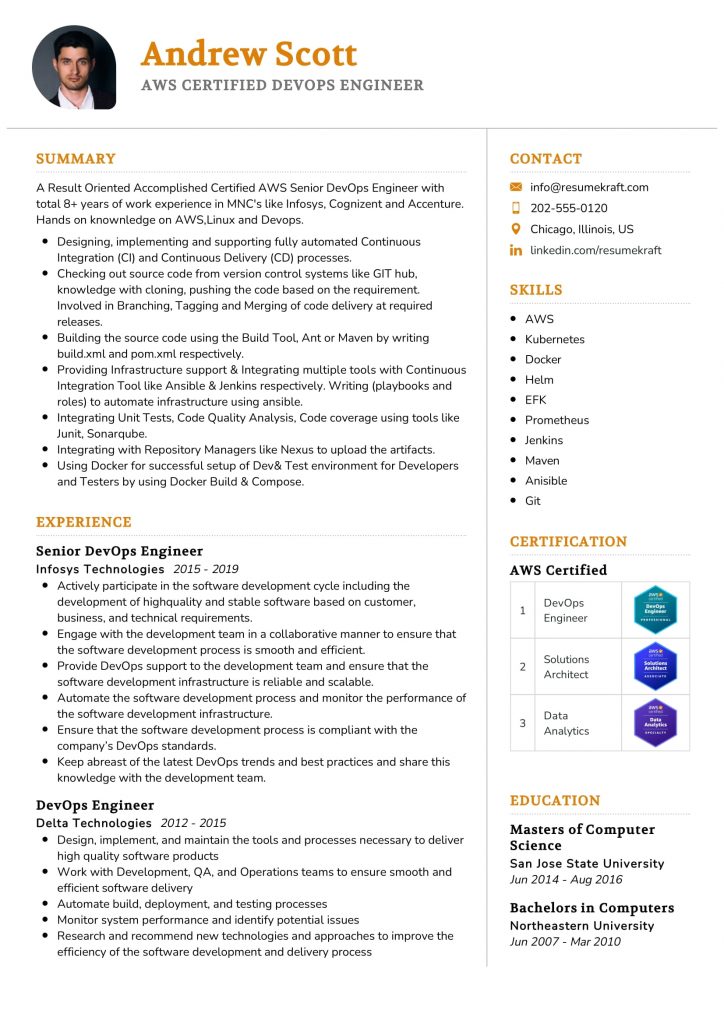
Build your resume in 5 minutes
Our resume builder is easy to use and will help you create a resume that is ATS-friendly and will stand out from the crowd.
40. What leadership qualities do you believe are essential for a Nurse Practitioner?
Essential leadership qualities for a Nurse Practitioner include effective communication, empathy, and the ability to inspire and mentor others. A good leader also demonstrates accountability and adaptability, ensuring that the team can navigate challenges. By cultivating a supportive environment, I can empower colleagues to excel, ultimately enhancing patient care.
41. Describe your experience with quality improvement initiatives in a clinical setting.
I have actively participated in several quality improvement initiatives focused on reducing patient readmission rates. By analyzing data and identifying trends, we implemented evidence-based protocols for discharge planning and patient education. These initiatives resulted in a measurable decrease in readmissions and improved patient satisfaction, demonstrating the importance of quality improvement in healthcare.
42. How do you stay updated with the latest medical research and advancements?
I stay updated with the latest medical research through various channels, including professional journals, online courses, and medical conferences. I also engage with professional organizations and participate in peer discussions to exchange knowledge and insights. This commitment to continuous learning ensures that my practice remains current and evidence-based, ultimately benefiting my patients.
How to Prepare for Your Nurse Practitioner Interview
Preparing for a Nurse Practitioner interview requires a strategic approach to showcase your clinical expertise, interpersonal skills, and understanding of healthcare dynamics. Focusing on specific areas can help you present yourself as a competent and confident candidate.
- Familiarize Yourself with the Role: Understand the specific responsibilities and scope of practice for Nurse Practitioners in the hiring institution. Review job descriptions and highlight key skills and experiences that align with their expectations.
- Review Common Interview Questions: Prepare for typical questions such as those about clinical scenarios, ethical dilemmas, and patient care strategies. Practice your responses to ensure clarity and confidence during the interview.
- Highlight Your Clinical Experience: Be ready to discuss your relevant clinical experiences, including specific patient populations you’ve worked with. Use the STAR method (Situation, Task, Action, Result) to effectively communicate your accomplishments.
- Prepare Your Questions: Have thoughtful questions ready for your interviewers about the practice environment, team dynamics, and professional development opportunities. This shows your genuine interest and helps you assess if the position is a good fit.
- Stay Updated on Healthcare Trends: Research current issues and trends in healthcare, particularly those affecting Nurse Practitioners. Being knowledgeable about industry changes demonstrates your commitment to continued learning and professional growth.
- Practice Professional Communication: Enhance your verbal and non-verbal communication skills by conducting mock interviews with peers or mentors. Focus on maintaining eye contact, a confident tone, and clear articulation of your thoughts.
- Dress Appropriately: Choose professional attire that reflects the standards of the healthcare setting. Dressing appropriately not only boosts your confidence but also creates a positive first impression with the interview panel.
Common Nurse Practitioner Interview Mistakes to Avoid
Preparing for a Nurse Practitioner interview can be challenging. Understanding common mistakes can help candidates present themselves more effectively, showcasing their skills and experience while making a positive impression on potential employers.
- Not Researching the Employer: Failing to understand the healthcare facility’s values and mission can make candidates appear disinterested. Researching the organization shows commitment and helps tailor responses to align with the employer’s goals.
- Neglecting Clinical Knowledge: Inadequate preparation on clinical guidelines or the latest evidence-based practices can hinder a candidate’s confidence. Being well-versed in relevant medical knowledge is crucial for demonstrating competence and expertise.
- Overlooking Behavioral Questions: Many interviews include behavioral questions to assess soft skills. Ignoring this aspect can lead to missed opportunities to showcase critical thinking, teamwork, and communication skills essential for patient care.
- Failing to Prepare Questions: Not asking questions at the end of the interview can signal a lack of interest. Thoughtful questions about patient care, team dynamics, or professional development show engagement and genuine interest in the role.
- Inadequate Self-Presentation: Poor attire or lack of professionalism can leave a negative impression. Dressing appropriately and maintaining good hygiene demonstrates respect for the interview process and the profession.
- Being Unprepared for Scenario Questions: Nurse Practitioner interviews often include hypothetical patient scenarios. Candidates should practice responding to these questions to showcase their clinical reasoning and ability to handle real-life situations effectively.
- Not Highlighting Unique Experiences: Failing to discuss unique experiences, such as volunteer work or specialized training, can lead to missed opportunities to stand out. Candidates should emphasize diverse experiences that enhance their qualifications.
- Neglecting Follow-Up: Forgetting to send a thank-you note after the interview can diminish a candidate’s chances. A follow-up note shows appreciation and reinforces interest in the position, keeping the candidate top-of-mind for the interviewer.
Key Takeaways for Nurse Practitioner Interview Success
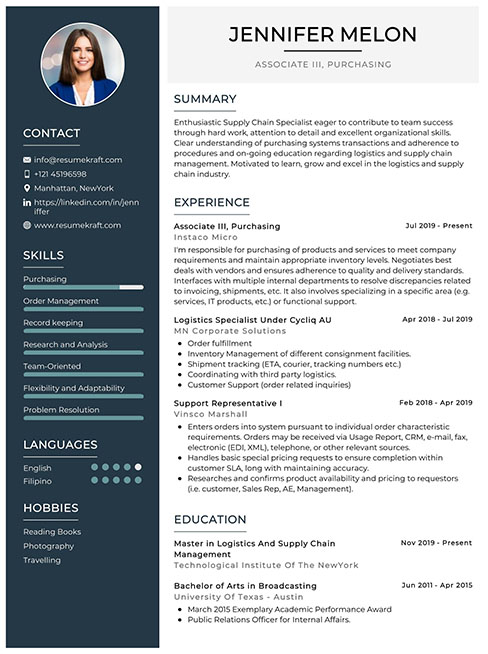
- Prepare a polished resume using AI resume builder tools to ensure clarity and professionalism. Choose appropriate resume templates that fit your experience to make a strong first impression.
- Showcase your experience effectively by referring to relevant resume examples tailored for nurse practitioners. Highlight specific skills and accomplishments that demonstrate your expertise in patient care.
- Craft personalized cover letters that align with the job description. This will help convey your passion for nursing and your understanding of the role, making your application stand out.
- Engage in mock interview practice to build confidence and refine your answers. This will help you articulate your qualifications and respond to common interview questions effectively.
- Research the healthcare facility and its values to tailor your responses. Understanding their mission will allow you to express how your goals align with their priorities during the interview.
Frequently Asked Questions
1. How long does a typical Nurse Practitioner interview last?
A typical Nurse Practitioner interview usually lasts between 30 minutes to an hour. This timeframe allows interviewers to assess your clinical knowledge, interpersonal skills, and fit within the team. During the interview, expect questions related to your clinical experiences, patient care strategies, and how you handle difficult situations. It’s important to be prepared for both situational and behavioral questions, as well as to have your own questions ready about the role and the organization.
2. What should I wear to a Nurse Practitioner interview?
For a Nurse Practitioner interview, it’s best to dress in professional attire that reflects the medical environment. Opt for business casual outfits, such as tailored slacks and a blouse or a blazer, which convey professionalism while still being comfortable. Avoid overly casual clothing like jeans or sneakers. Make sure your appearance is neat and polished, as first impressions are crucial in healthcare settings. Additionally, consider the organization’s culture when selecting your outfit to ensure it aligns.
3. How many rounds of interviews are typical for a Nurse Practitioner position?
Typically, a Nurse Practitioner position may involve two to three rounds of interviews. The first round is often with a recruiter or HR representative to discuss your qualifications and fit for the role. Subsequent interviews may be with hiring managers or clinical teams, focusing on your clinical skills and case scenarios. In some cases, a final interview may include a panel or a practical assessment. Each round is an opportunity to showcase your expertise and interpersonal skills.
4. Should I send a thank-you note after my Nurse Practitioner interview?
Yes, sending a thank-you note after your Nurse Practitioner interview is highly recommended. It shows your appreciation for the opportunity and reinforces your interest in the position. Aim to send the note within 24 hours of the interview, either via email or a handwritten card, depending on the organization’s culture. In your note, briefly express gratitude, mention specific topics discussed, and reiterate your enthusiasm for the role. This gesture can leave a lasting positive impression.