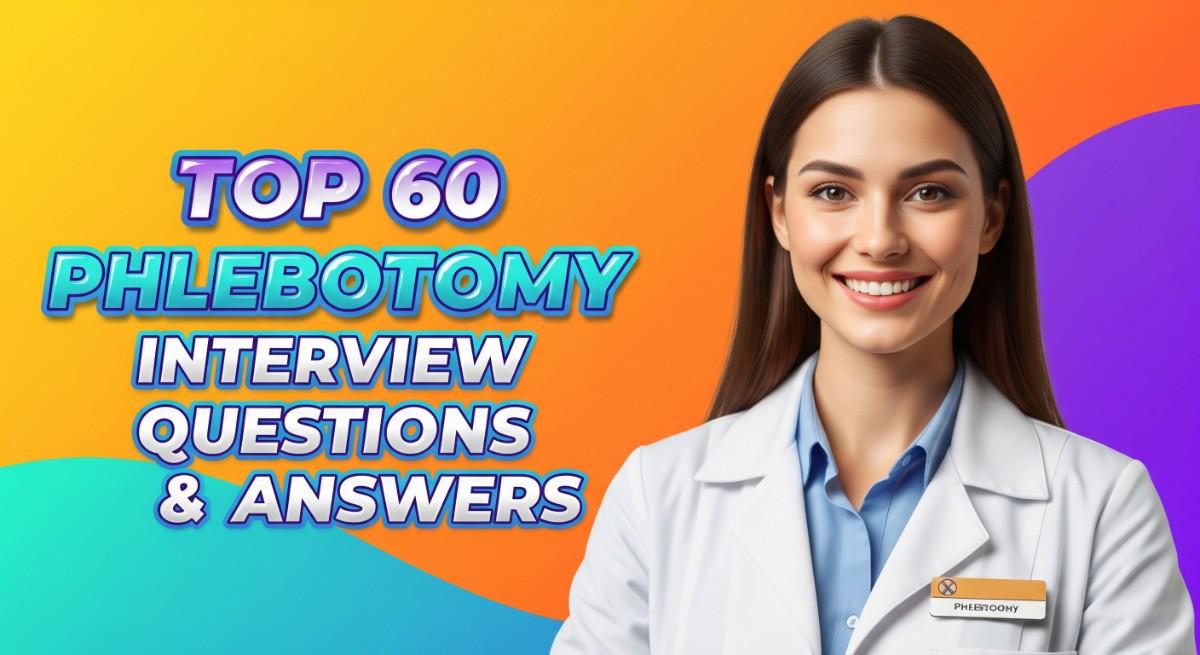
Preparing for a phlebotomy interview is a crucial step in entering this rewarding healthcare profession. Phlebotomists play a vital role in patient care, as they are responsible for drawing blood and ensuring accurate sample collection for diagnostic testing. This unique position requires not only technical skills but also strong interpersonal abilities, as you will interact with patients and medical staff alike. Proper interview preparation is essential to showcase your expertise and confidence. In this comprehensive guide, we will cover common interview questions, effective strategies for answering them, tips for presenting your skills and experience, and ways to demonstrate your passion for phlebotomy.
What to Expect in a Phlebotomy Interview
In a Phlebotomy interview, candidates can expect a mix of behavioral and technical questions aimed at assessing their skills and knowledge in blood collection and patient care. Interviews are typically conducted by hiring managers, lab supervisors, or experienced phlebotomists. The process usually starts with general questions about the candidate’s background and experience, followed by situational questions that evaluate problem-solving abilities. Candidates may also be asked about safety protocols, handling difficult patients, and their familiarity with lab equipment. Practical assessments or role-playing scenarios may be included to gauge hands-on skills.
Phlebotomy Interview Questions For Freshers
This set of Phlebotomy interview questions is designed for freshers entering the field. Candidates should master fundamental concepts such as blood collection techniques, safety protocols, and patient interaction to demonstrate their readiness for the role.
1. What is phlebotomy?
Phlebotomy is the practice of drawing blood from patients for clinical or medical testing, transfusions, donations, or research. Phlebotomists are trained to perform this task safely and efficiently while ensuring patient comfort and adhering to strict health regulations. Their role is crucial in the healthcare system for diagnostics and treatment monitoring.
2. What are the key responsibilities of a phlebotomist?
- Blood Collection: Perform venipunctures, capillary punctures, and other methods to collect blood samples.
- Patient Interaction: Explain the procedure to patients, ensuring their comfort and addressing any concerns.
- Sample Handling: Properly label and handle blood samples to prevent contamination and ensure accurate testing.
- Safety Protocols: Follow infection control practices and dispose of biohazard waste according to regulations.
These responsibilities highlight the importance of technical skills as well as interpersonal communication in the role of a phlebotomist.
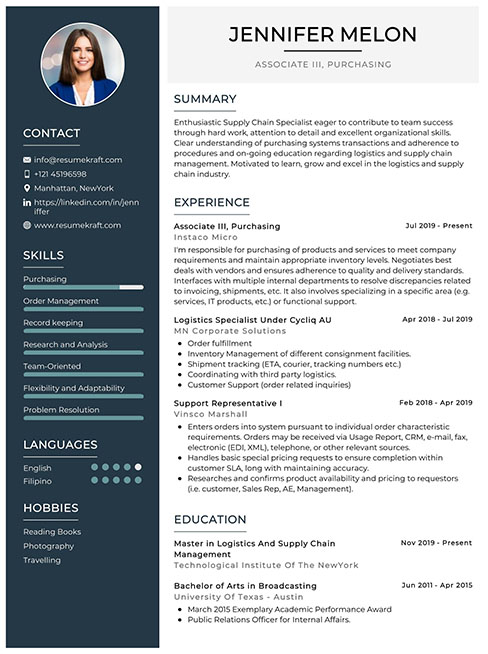
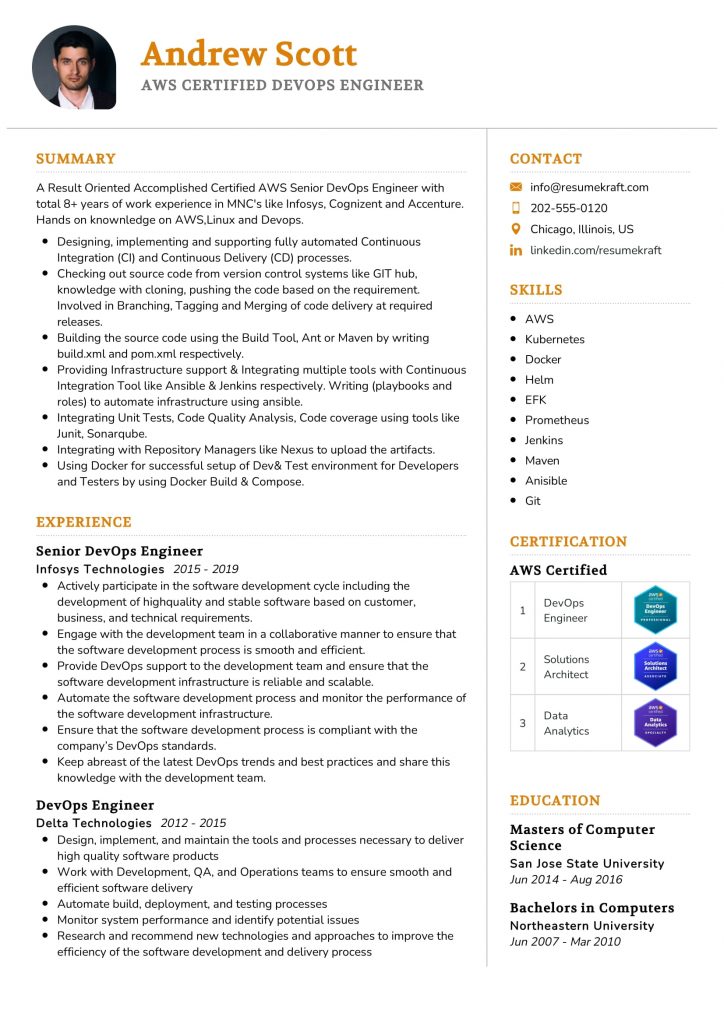
Build your resume in just 5 minutes with AI.
3. What equipment is commonly used in phlebotomy?
Common equipment used in phlebotomy includes tourniquets, alcohol wipes, needles, vacutainers, and gauze. Tourniquets are used to engorge veins, making them more visible. Alcohol wipes help disinfect the puncture site, while vacutainers are used to collect and store blood samples in specific tubes for various tests.
4. How do you ensure patient safety during a blood draw?
- Informed Consent: Always explain the procedure and obtain verbal or written consent from the patient.
- Hygiene: Use gloves and maintain a sterile environment to prevent infection.
- Comfort: Make the patient comfortable and relaxed to reduce anxiety and improve vein visibility.
- Post-Procedure Care: Apply pressure and a bandage to the puncture site to minimize bleeding.
By following these practices, a phlebotomist can ensure the safety and well-being of their patients.
5. What are the different methods of blood collection?
- Venipuncture: Involves inserting a needle into a vein, usually in the arm, to draw blood.
- Capillary Puncture: A small puncture is made in the skin, typically on a fingertip or heel, to collect a few drops of blood.
- Arterial Collection: Involves drawing blood from an artery, usually for blood gas analysis.
Understanding these methods is essential for phlebotomists to choose the appropriate technique based on the patient’s needs and the required tests.
6. What is the role of the tourniquet in phlebotomy?
The tourniquet is used to temporarily restrict blood flow in the veins, making them more prominent and easier to access for venipuncture. It is typically applied a few inches above the intended puncture site and should be released as soon as the blood collection is initiated to prevent complications such as hematoma formation.
7. How do you handle difficult veins?
- Palpation: Use your fingers to feel for veins that are deeper or less visible.
- Warm Compress: Apply a warm cloth to the area to dilate veins and improve visibility.
- Repositioning: Adjust the patient’s position or ask them to make a fist to enhance vein prominence.
- Alternative Sites: Consider using other sites such as the hand or wrist if necessary.
These strategies can help improve the chances of a successful blood draw in patients with difficult veins.
8. What precautions are necessary for infection control?
- Hand Hygiene: Wash hands thoroughly before and after patient contact and blood draws.
- Use of Gloves: Always wear disposable gloves to protect both the patient and phlebotomist.
- Disinfection: Clean the puncture site with an appropriate antiseptic solution before the procedure.
- Safe Disposal: Dispose of needles and other sharp objects in designated biohazard containers.
Implementing these precautions is vital for maintaining a safe and sterile environment in healthcare settings.
9. What steps do you take if a patient faints during a blood draw?
- Stop the Procedure: Immediately cease the blood draw to ensure the patient’s safety.
- Positioning: Lay the patient down flat to increase blood flow to the brain.
- Monitor: Keep an eye on their breathing and pulse until they regain consciousness.
- Provide Support: Offer water or juice once they are alert to help restore their energy.
Being prepared for such situations ensures that phlebotomists can effectively manage patient reactions during blood draws.
10. Can you explain the proper labeling of blood samples?
Proper labeling of blood samples is essential for accurate testing and includes the patient’s name, identification number, date and time of collection, and the type of test ordered. Labels should be affixed to the sample tube immediately after collection to avoid mix-ups and ensure traceability throughout the testing process.
11. What is the significance of the order of draw in phlebotomy?
The order of draw refers to the sequence in which different blood collection tubes should be filled to prevent cross-contamination of additives between tubes. For example, blood cultures should be drawn first, followed by light blue, red, green, and lavender tubes. Adhering to this order ensures accurate test results and prevents erroneous findings.
12. How do you handle a situation where a patient refuses to have their blood drawn?
In such cases, it’s important to respect the patient’s decision while ensuring they are fully informed about the implications of refusing the procedure. Engage the patient in a conversation, addressing their concerns and providing information on the importance of the test. If they still refuse, document the refusal and inform the supervising healthcare provider.
13. What are some common complications that can occur during a blood draw?
- Hematoma: Accumulation of blood outside the vessel, causing swelling and pain.
- Phlebitis: Inflammation of the vein that can occur after multiple punctures.
- Infection: A risk if proper aseptic techniques are not followed.
- Vasovagal Syncope: A fainting response that may occur in some patients during or after the procedure.
Understanding these complications helps phlebotomists take preventive measures and manage any issues that arise effectively.
14. What is the difference between serum and plasma?
Serum is the liquid portion of blood that remains after clotting has occurred, while plasma is the liquid component of blood that includes clotting factors and is obtained by centrifuging whole blood without allowing it to clot. This distinction is important as different tests require either serum or plasma for accurate results.
15. Why is patient identification crucial in phlebotomy?
Patient identification is crucial to ensure that blood samples are accurately matched to the correct patient for testing. Misidentification can lead to incorrect test results, misdiagnosis, and inappropriate treatment. Therefore, verifying the patient’s identity through multiple identifiers, such as name and date of birth, is a standard practice in phlebotomy.
These questions are tailored for freshers entering the phlebotomy field and cover essential concepts they should be familiar with.
16. What is phlebotomy and what role does a phlebotomist play?
Phlebotomy is the practice of drawing blood from patients for medical testing, transfusions, research, or donations. A phlebotomist is a trained professional responsible for this procedure. Their role includes preparing patients for blood draws, ensuring the correct collection and labeling of samples, maintaining sterile techniques to prevent infection, and sometimes performing preliminary tests on the samples collected. They must also have good communication skills to explain the process to patients and alleviate any concerns.
17. What are the different types of blood collection methods?
- Venipuncture: This is the most common method, where blood is drawn from a vein, usually in the arm, using a needle and a vacuum tube.
- Capillary collection: This method is used for small blood samples, typically from infants, where blood is taken from a fingerstick or heelstick.
- Arterial collection: This is less common and is performed to measure blood gases, where blood is drawn from an artery.
Each method has specific indications and is chosen based on the patient’s condition and the tests required.
18. Why is it important to properly identify a patient before drawing blood?
Proper patient identification is crucial in phlebotomy to ensure the accuracy of lab results and patient safety. Misidentification can lead to incorrect diagnoses, inappropriate treatments, and potential harm to the patient. It typically involves confirming the patient’s name, date of birth, and often using an identification band when available. This process is essential to maintain the integrity of the sample and the patient’s medical records.
19. What are the common complications associated with phlebotomy?
- Hematoma: This occurs when blood leaks into the tissue around the puncture site, causing swelling and bruising.
- Infection: There is a risk of infection if sterile techniques are not followed during the blood draw.
- Syncope: Some patients may faint during or after the procedure due to anxiety or the sight of blood.
Being aware of these complications helps phlebotomists take preventive measures and respond effectively if they occur.
20. What is the significance of using the correct order of draw for blood collection?
The order of draw refers to the sequence in which blood collection tubes should be filled to prevent cross-contamination of additives. The correct order helps ensure accurate test results by avoiding chemical interactions between different additives in the tubes. Typically, the order starts with blood cultures, followed by blue-top tubes for coagulation studies, and then other colored tubes depending on their specific additives. Following the correct sequence is a key responsibility for phlebotomists.
21. How should a phlebotomist handle a patient who is anxious about the blood draw?
When dealing with an anxious patient, a phlebotomist should use a calm and reassuring approach. This can include explaining the procedure in simple terms, addressing any concerns, and ensuring the patient feels comfortable throughout the process. Offering to have a discussion about what to expect can help ease anxiety. Additionally, employing techniques such as distraction or deep-breathing exercises can help manage the patient’s stress levels during the blood draw.
Phlebotomy Intermediate Interview Questions
Phlebotomy interview questions for intermediate candidates focus on practical skills, safety protocols, and patient interaction techniques. Candidates should be familiar with blood collection methods, common challenges in the field, and best practices to ensure accuracy and patient comfort during procedures.
22. What are the different blood collection methods used in phlebotomy?
In phlebotomy, the primary blood collection methods include venipuncture, capillary puncture, and arterial puncture. Venipuncture is the most common technique, involving the insertion of a needle into a vein to draw blood. Capillary puncture is used for small blood samples, typically from infants or when only a few drops are needed. Arterial puncture is less common and is used to measure blood gases, requiring a more skilled approach due to the risks involved.
23. How do you ensure patient safety during a blood draw?
- Informed consent: Always explain the procedure to the patient and obtain their consent.
- Proper identification: Verify the patient’s identity using their wristband or other identification methods to prevent mix-ups.
- Hygiene practices: Use gloves, sanitize the site, and follow infection control protocols to minimize the risk of contamination.
Ensuring patient safety is paramount in phlebotomy, as it helps to build trust and reduces the likelihood of complications.
24. What steps do you take if you encounter a difficult vein?
- Change position: Ask the patient to change positions or use a warm compress to dilate the veins.
- Use a smaller needle: Consider using a smaller gauge needle which might be less painful and easier to insert.
- Alternative sites: If necessary, look for other potential sites such as the hand or wrist.
These strategies can help improve the chances of a successful blood draw without causing undue discomfort to the patient.
25. What is the significance of the order of draw in phlebotomy?
The order of draw is crucial to prevent cross-contamination between different additives in blood collection tubes. This ensures accurate test results. The general order is: blood cultures, light blue (sodium citrate), red (no additive), gold or tiger top (serum separator), green (heparin), lavender (EDTA), and gray (fluoride). Following this order minimizes the risk of contamination that can affect laboratory results.
26. How do you handle a patient who is anxious about the blood draw?
- Reassurance: Communicate calmly and reassure the patient about the process.
- Distraction techniques: Use conversation or provide a stress ball to distract them during the draw.
- Explain the procedure: Providing information about what to expect can help ease their anxiety.
By addressing the patient’s concerns and creating a supportive environment, you can help them feel more comfortable during the procedure.
27. What are the potential complications of phlebotomy?
- Hematoma: This occurs when blood leaks into the surrounding tissue, causing swelling and discoloration.
- Phlebitis: Inflammation of the vein can occur, leading to pain and redness at the site.
- Infection: There’s a risk of introducing bacteria into the bloodstream if proper aseptic techniques are not followed.
Awareness of these complications allows phlebotomists to take preventive measures and address issues promptly if they arise.
28. What is the role of additives in blood collection tubes?
Additives in blood collection tubes serve specific purposes depending on the tests to be performed. For example, anticoagulants like EDTA prevent coagulation for hematology tests, while serum separator tubes contain a gel that facilitates the separation of serum from cells after centrifugation. Understanding the role of these additives is essential for obtaining accurate test results and proper specimen handling.
29. How do you ensure proper labeling of blood samples?
- Immediate labeling: Label samples immediately at the bedside after collection to avoid mix-ups.
- Include key information: Ensure labels contain the patient’s name, date of birth, date and time of collection, and the type of test requested.
- Use barcodes: Whenever possible, utilize barcode systems to automate and verify patient information.
Proper labeling is vital for maintaining the integrity of the samples and ensuring accurate test results.
30. What techniques can be used to minimize pain during a blood draw?
- Use of a smaller needle: A smaller gauge needle can reduce discomfort for the patient.
- Topical anesthetic: Application of a topical anesthetic cream can numb the area before the draw.
- Proper technique: Ensure that the needle is inserted at the correct angle and depth to minimize pain.
Implementing these techniques can significantly enhance the comfort level of patients during blood collection.
31. How do you manage a situation where a patient faints during a blood draw?
- Immediate response: Stop the draw and help the patient to a lying position to prevent injury.
- Assess vitals: Monitor the patient’s pulse and breathing, and provide oxygen if necessary.
- Reassure and hydrate: Once stable, reassure the patient and offer water or juice to help recover.
Being prepared to handle fainting can ensure patient safety and comfort during the procedure.
32. What are the best practices for disposing of sharps?
Sharps must be disposed of in puncture-resistant containers that are clearly labeled and located within reach. Never overfill these containers; they should be sealed when three-quarters full. Regularly check for compliance with local regulations regarding sharps disposal to ensure safety and environmental protection.
33. Can you explain the process of capillary blood collection?
Capillary blood collection involves pricking the skin, usually on the fingertip or heel, to obtain a small sample of blood. The site is cleaned with an alcohol swab, and after drying, a lancet is used to puncture the skin. Blood is then collected using a micro-collection tube or capillary tube. This method is often used for pediatric patients or when only a small sample is needed.
34. How do you handle and transport blood specimens?
- Maintain temperature: Ensure specimens are transported at the appropriate temperature, depending on the test requirements.
- Protect from light: Some tests require samples to be protected from light, so use opaque containers when necessary.
- Timely delivery: Transport samples to the laboratory as quickly as possible to minimize degradation.
Proper handling and transportation of blood specimens are critical to ensuring the reliability of test results.
35. What information should be included in a phlebotomy report?
A phlebotomy report should include patient demographics (name, ID, date of birth), details of the blood draw (date, time, site), type of samples collected, and any relevant notes regarding the procedure or patient’s condition. This information is essential for laboratory processing and clinical correlation.
Below are intermediate interview questions for phlebotomy that cover practical applications and best practices in the field.
37. What are the most common complications that can arise during phlebotomy?
Complications during phlebotomy can include:
- Hematoma: This occurs when blood leaks into the tissue surrounding the vein, causing swelling and discoloration.
- Phlebitis: Inflammation of the vein can occur due to irritation from the needle or the collection process.
- Infection: There is a risk of introducing pathogens at the puncture site, leading to localized infections.
- Vasovagal reaction: Some patients may faint due to anxiety or the sight of blood.
Understanding these complications helps phlebotomists prepare and respond effectively to ensure patient safety.
38. How do you ensure proper patient identification before a blood draw?
Proper patient identification is crucial in phlebotomy to prevent errors. The following steps should be taken:
- Ask the patient to state their full name and date of birth, and verify this information against their wristband.
- Use two identifiers, such as the patient’s name and medical record number, to confirm their identity.
- Ensure that the identification process is documented in the patient’s medical record.
This method minimizes the risk of misidentification and ensures accurate lab results.
39. What is the proper order of draw for blood collection tubes, and why is it important?
The order of draw is crucial to prevent cross-contamination of additives between tubes. The recommended order is:
- Blood culture bottles or tubes
- Coagulation tubes (e.g., blue top)
- Serum tubes (e.g., red or gold top)
- Heparin tubes (e.g., green top)
- EDTA tubes (e.g., lavender top)
- Glycolytic inhibitor tubes (e.g., gray top)
Following this order ensures that the results from different tests are reliable and accurate.
40. Describe the techniques used for vein selection in phlebotomy.
Vein selection is critical for a successful blood draw. Techniques include:
- Visual inspection: Look for prominent veins in the antecubital fossa or back of the hand.
- Palpation: Feel for a vein’s elasticity and depth, ensuring it’s suitable for puncture.
- Use of heat: Applying a warm compress can dilate veins, making them easier to locate.
- Gravity: Instructing the patient to lower their arm can help fill the veins with blood.
Choosing the right vein enhances the success of the procedure and minimizes discomfort for the patient.
41. What are the steps to take if a patient has a vasovagal reaction during a blood draw?
If a patient experiences a vasovagal reaction, follow these steps:
- Stop the blood draw immediately and remove the needle.
- Help the patient into a lying position to improve blood flow to the brain.
- Elevate their legs, if possible, to facilitate circulation.
- Monitor the patient’s condition and provide cool cloths or water as needed.
Being prepared for such reactions ensures patient safety and comfort during the procedure.
42. How do you handle and dispose of sharp instruments in phlebotomy?
Handling and disposing of sharp instruments is critical for safety. The following practices should be followed:
- Always use a safety-engineered device when available to minimize the risk of needlestick injuries.
- Immediately dispose of used needles and sharp instruments in designated sharps containers to prevent injuries.
- Ensure that the sharps container is puncture-resistant, labeled, and located within reach.
- Do not recap needles after use, as this increases the risk of injury.
Adhering to these practices protects both healthcare workers and patients from potential harm.
Phlebotomy Interview Questions for Experienced
This set of Phlebotomy interview questions is tailored for experienced professionals, focusing on advanced topics such as best practices in blood collection, management of complex cases, regulatory compliance, and mentoring techniques in the field. These questions aim to assess both technical knowledge and leadership abilities.
43. What are the key considerations for ensuring patient safety during phlebotomy procedures?
Ensuring patient safety during phlebotomy is paramount. Key considerations include:
- Proper identification: Always confirm the patient’s identity using two identifiers.
- Infection control: Use aseptic techniques and appropriate personal protective equipment (PPE) to minimize infection risk.
- Correct technique: Employ the right venipuncture technique to reduce pain and prevent complications.
- Monitoring: Observe the patient for any adverse reactions during and after the procedure.
These practices help maintain high standards of patient care and reduce the likelihood of errors.
Build your resume in 5 minutes
Our resume builder is easy to use and will help you create a resume that is ATS-friendly and will stand out from the crowd.
44. How do you handle difficult patients or those with a fear of needles?
Handling difficult patients requires empathy and effective communication. Strategies include:
- Build rapport: Start with a friendly conversation to ease anxiety.
- Explain the procedure: Clearly describe what will happen and how it will feel.
- Distraction techniques: Use visual or auditory distractions to divert attention during the procedure.
- Involve support: Encourage the presence of a family member or friend for comfort.
These approaches can significantly improve the patient’s experience and cooperation.
45. Can you describe your experience with different types of blood collection techniques?
I have experience with various blood collection techniques, including:
- Venipuncture: This is the most common method, using a needle to access a vein for blood sampling.
- Capillary collection: Used for infants and patients with difficult venous access, involving a small puncture in the skin.
- Arterial sampling: This technique is used for specific tests that require arterial blood, such as blood gas analysis.
Each technique has its indications, and proper selection is key to successful blood collection.
46. What measures do you take to maintain the integrity of blood samples?
Maintaining the integrity of blood samples involves several critical measures:
- Correct labeling: Ensure samples are accurately labeled at the time of collection to prevent mix-ups.
- Proper storage: Adhere to temperature and storage guidelines based on the type of specimen.
- Timely transport: Samples should be delivered to the lab as soon as possible to prevent degradation.
- Contamination avoidance: Use sterile techniques and equipment to prevent contamination during collection.
These practices are essential for reliable test results.
47. How do you stay updated on regulatory compliance and best practices in phlebotomy?
Staying updated on regulatory compliance involves several proactive approaches:
- Continuing education: Attend workshops, seminars, and certification programs to enhance knowledge.
- Professional organizations: Join organizations like the American Society for Clinical Laboratory Science (ASCLS) for resources and networking.
- Policy updates: Regularly review updates from regulatory bodies such as the CDC and OSHA.
- Peer discussions: Engage in discussions with colleagues to share insights and experiences.
These efforts help ensure compliance and improve practice standards.
48. Describe a challenging case you’ve encountered in phlebotomy and how you handled it.
In one instance, I encountered a patient with a history of difficult venous access. To address this, I first assessed their veins visually and palpated to find the best site. I then explained the situation to the patient and offered them options, such as using a butterfly needle for better control. After successfully collecting the sample, I ensured to document the procedure and inform the lab of the challenges faced. This approach minimized discomfort and built trust with the patient.
49. What role does technology play in modern phlebotomy practices?
Technology plays a significant role in enhancing phlebotomy practices, including:
- Automated blood collection systems: These devices can streamline the collection process, reducing errors.
- Electronic health records (EHR): EHRs facilitate accurate documentation and tracking of patient information and samples.
- Mobile phlebotomy apps: These applications help schedule appointments and manage patient data efficiently.
- Training simulators: Virtual reality and simulation tools are increasingly used for training new phlebotomists.
Overall, technology improves efficiency, accuracy, and patient care quality.
50. How do you approach mentoring new phlebotomists in your team?
Mentoring new phlebotomists involves a structured approach:
- Initial assessment: Evaluate their skills and knowledge to tailor the mentorship accordingly.
- Hands-on training: Provide practical experience under supervision, gradually increasing independence.
- Regular feedback: Offer constructive feedback on techniques and patient interactions to foster improvement.
- Encourage questions: Create an open environment where mentees feel comfortable asking questions.
This method not only builds their confidence but also enhances team competence.
51. What techniques do you use to minimize patient discomfort during procedures?
To minimize patient discomfort during phlebotomy, I employ several techniques:
- Use smaller gauge needles: This can reduce pain during venipuncture.
- Warm compresses: Applying a warm compress to the site prior to puncture can help dilate veins.
- Proper positioning: Ensure the patient is comfortable and relaxed to reduce tension.
- Gentle technique: Use a swift and confident approach when inserting the needle.
These techniques contribute to a more positive patient experience.
52. How do you handle phlebotomy in patients with special needs or disabilities?
Handling phlebotomy for patients with special needs requires adaptability and sensitivity:
- Assessment: Evaluate the patient’s specific needs and challenges prior to the procedure.
- Communication: Clearly explain the procedure and obtain consent, using appropriate communication methods.
- Assistance: Involve caregivers or family members for support and guidance during the procedure.
- Modified techniques: Adjust techniques and equipment based on the patient’s condition.
This ensures the procedure is as comfortable and efficient as possible for the patient.
53. What are the most common complications you encounter in phlebotomy, and how do you manage them?
Common complications in phlebotomy include:
- Hematoma: This occurs when blood leaks into surrounding tissues. To manage it, apply pressure and elevate the site.
- Phlebitis: Inflammation of the vein can occur. If suspected, avoid using the affected vein for future collections.
- Syncope: Fainting may happen, especially in anxious patients. Monitor them and lay them down until they recover.
- Infection: If an infection is suspected, notify medical staff and ensure proper wound care.
Awareness and prompt management of these complications are essential for patient safety.
54. How do you ensure effective communication with other healthcare professionals regarding patient samples?
Effective communication with healthcare professionals is critical for patient care. Strategies include:
- Clear documentation: Ensure all sample details are accurately recorded and easily accessible.
- Timely updates: Inform relevant staff promptly about any issues or changes regarding samples.
- Interdisciplinary meetings: Participate in regular meetings to discuss patient care and sample handling.
- Use of EHR: Utilize electronic health records to facilitate communication and track samples efficiently.
These practices enhance collaboration and ensure high-quality patient care.
55. What is your experience with managing phlebotomy services in a high-volume environment?
In a high-volume environment, managing phlebotomy services involves:
- Efficient scheduling: Implement a streamlined appointment system to reduce wait times.
- Staff training: Ensure all staff are well-trained to handle increased patient flow without compromising quality.
- Workflow optimization: Regularly assess and improve workflows to enhance efficiency.
- Quality control: Establish protocols to maintain high standards despite the volume of samples collected.
These strategies are essential for maintaining service quality in busy settings.
These questions are designed for experienced phlebotomists and cover advanced topics relevant to their roles, including procedure optimization, patient interaction, and leadership in the clinical environment.
58. How do you ensure proper patient identification before performing a venipuncture?
Ensuring proper patient identification is critical to avoid errors in sample collection. The standard protocol involves:
- Using two unique patient identifiers: Typically, this includes the patient’s full name and date of birth.
- Verifying information through wristbands: If available, check the patient’s wristband against the requisition form.
- Asking the patient to confirm their details: This engages the patient and provides an additional layer of verification.
Implementing these steps helps maintain patient safety and ensures the integrity of the lab results.
59. What strategies do you use to manage difficult patients during blood draws?
Managing difficult patients requires patience and effective communication. Here are key strategies:
- Establish rapport: Take a moment to introduce yourself and explain the procedure to alleviate anxiety.
- Use calming techniques: Speak in a soothing tone and offer reassurance throughout the procedure.
- Be adaptable: Modify the approach based on the patient’s reactions, such as taking breaks if they feel overwhelmed.
These strategies not only improve the patient experience but also enhance the likelihood of a successful blood draw.
60. Can you describe a time when you had to mentor a less experienced phlebotomist? What approach did you take?
Mentoring a less experienced phlebotomist involves guiding them through practical skills and fostering their confidence. In one instance, I paired with a new hire and took the following approach:
- Hands-on demonstrations: I first demonstrated venipuncture techniques, explaining each step clearly.
- Encouragement of questions: I created an open environment where they felt comfortable asking questions and discussing concerns.
- Gradual independence: I allowed them to perform procedures under supervision, providing constructive feedback while encouraging their decision-making.
This method not only helped the new phlebotomist develop their skills but also promoted a supportive team culture.
How to Prepare for Your Phlebotomy Interview
Preparing for a Phlebotomy interview requires a blend of technical knowledge, practical skills, and effective communication. Familiarizing yourself with common interview questions, practicing your responses, and understanding the role’s responsibilities will enhance your confidence and performance on interview day.
- Research the Employer: Understand the facility’s mission, values, and patient demographics. Familiarizing yourself with the organization can help you tailor your responses and demonstrate your interest in their specific practices and culture during the interview.
- Review Phlebotomy Techniques: Brush up on your knowledge of venipuncture, capillary punctures, and proper specimen handling. Be prepared to discuss these techniques in detail, as interviewers may ask for your approach to different scenarios in a clinical setting.
- Prepare for Behavioral Questions: Anticipate questions about teamwork, conflict resolution, and patient care. Use the STAR method (Situation, Task, Action, Result) to structure your answers, providing clear examples from your training or previous experiences.
- Practice Your Communication Skills: Phlebotomists often interact with patients, so practice explaining procedures clearly and reassuringly. Role-play with a friend to enhance your verbal communication and ensure you can convey information confidently and compassionately.
- Familiarize Yourself with Safety Protocols: Know the key safety and infection control measures in phlebotomy. Be prepared to discuss your understanding of OSHA regulations, proper disposal of sharps, and how to maintain a sterile environment.
- Dress Professionally: First impressions matter. Wear professional attire that aligns with the healthcare environment. Ensure your appearance is neat and polished, as this reflects your seriousness about the position and your respect for the interviewers.
- Prepare Questions to Ask: Have thoughtful questions ready to ask the interviewer about the role, team dynamics, and training opportunities. This shows your interest in the position and helps you assess if the organization is the right fit for you.
Common Phlebotomy Interview Mistakes to Avoid
Preparing for a Phlebotomy interview is crucial for success. Many candidates make common mistakes that can hinder their chances. Understanding these pitfalls can help you present yourself more effectively and demonstrate your qualifications for the role.
- Not demonstrating technical skills: Phlebotomy requires specific technical abilities. Failing to discuss your hands-on experience with venipuncture and specimen collection can raise concerns about your competency.
- Ignoring safety protocols: Safety is paramount in phlebotomy. Candidates should discuss their knowledge of infection control, proper disposal of sharps, and adherence to OSHA regulations to show their commitment to patient safety.
- Underestimating the importance of patient interaction: Phlebotomists must interact with patients regularly. Neglecting to mention your communication skills or experience in calming anxious patients can indicate a lack of understanding of the role’s interpersonal aspects.
- Not researching the employer: Failing to know about the healthcare facility or lab can make you seem unprepared. Understanding the company’s values, mission, and the services they offer shows genuine interest and initiative.
- Providing vague answers: When asked about your experiences, specific examples are essential. Vague responses can make it difficult for interviewers to gauge your qualifications and suitability for the position.
- Neglecting to ask questions: Not preparing thoughtful questions about the role or the organization can signal disinterest. Asking insightful questions demonstrates your enthusiasm and willingness to learn more about the position.
- Focusing too much on salary: While salary is important, emphasizing it during the interview may give the impression that you’re more interested in compensation than in providing quality patient care.
- Dressing inappropriately: First impressions matter. Dressing too casually can reflect poorly on your professionalism. Opt for business attire to convey seriousness about the position and respect for the interview process.
Key Takeaways for Phlebotomy Interview Success
- Prepare a polished resume using an AI resume builder to highlight your skills and experience effectively, ensuring it aligns with the specific requirements of the phlebotomy role.
- Utilize resume templates to create a well-structured document that emphasizes your educational background and relevant certifications, making it easier for employers to assess your qualifications.
- Showcase your experience with strong resume examples that demonstrate your practical skills in phlebotomy, including any internships or hands-on training you have completed.
- Craft tailored cover letters that express your passion for phlebotomy and explain why you are an ideal fit for the position, complementing your resume efforts.
- Engage in mock interview practice to refine your responses to common phlebotomy interview questions, helping you build confidence and improve your communication skills.
Frequently Asked Questions
1. How long does a typical Phlebotomy interview last?
A typical Phlebotomy interview lasts between 30 minutes to an hour. This timeframe allows the interviewer to assess your technical skills, knowledge of procedures, and ability to communicate effectively with patients. Be prepared to answer questions about your experience, certifications, and how you handle various situations in the lab or during patient interactions. It’s also an opportunity for you to ask questions about the workplace and team dynamics.
2. What should I wear to a Phlebotomy interview?
For a Phlebotomy interview, you should aim for business casual attire. This typically means wearing slacks or a knee-length skirt, a collared shirt, and closed-toe shoes. Avoid overly casual clothing such as jeans or sneakers. Dressing professionally demonstrates your respect for the opportunity and shows that you understand the importance of a polished appearance in a healthcare environment. Ensure your outfit is neat, clean, and comfortable to help you feel confident.
3. How many rounds of interviews are typical for a Phlebotomy position?
Generally, a Phlebotomy position may involve one to three rounds of interviews. The first round is often a screening interview conducted by HR, focusing on your qualifications and experience. Subsequent rounds may include interviews with the lab manager or lead phlebotomist, where you might be asked more technical questions or scenarios. Some facilities may also include a practical assessment to evaluate your skills directly. Be prepared for different formats and interviewers.
4. Should I send a thank-you note after my Phlebotomy interview?
Yes, sending a thank-you note after your Phlebotomy interview is highly recommended. It shows appreciation for the opportunity and reinforces your interest in the position. A brief, polite note can help you stand out from other candidates and leave a positive impression on the interviewers. In your note, express gratitude for their time, mention a specific topic discussed during the interview, and reiterate your enthusiasm for joining their team.