Preparing for a Certified Registered Nurse Anesthetist (CRNA) interview is a crucial step in advancing your career in anesthesia. This role is unique due to its blend of advanced nursing skills and specialized anesthetic knowledge, requiring a deep understanding of pharmacology, physiology, and patient management. Proper interview preparation not only helps you articulate your expertise but also boosts your confidence in showcasing your clinical experiences and decision-making abilities. This comprehensive guide will cover essential topics, including common interview questions, effective strategies for answering them, and tips on how to present your qualifications in the best light, ensuring you stand out as a strong candidate for this vital healthcare position.
What to Expect in a CRNA Interview
In a Certified Registered Nurse Anesthetist (CRNA) interview, candidates can expect a combination of behavioral and clinical questions, focusing on their experience, critical thinking, and decision-making skills. The interview may be conducted by a panel including anesthesiologists, CRNAs, and nurse leaders. Typically, the process starts with a brief introduction, followed by questions assessing clinical knowledge, patient scenarios, and teamwork abilities. Candidates may also discuss their motivation for pursuing anesthesia and their understanding of the role. This structured approach helps evaluate both technical skills and interpersonal qualities essential for the position.
CRNA Interview Questions For Freshers
This collection of CRNA interview questions is tailored for freshers entering the field. Mastering these fundamental concepts will prepare candidates for discussions around anesthesia principles, pharmacology, and patient care, ensuring they have a solid foundation for their upcoming interviews.
1. What is the role of a Certified Registered Nurse Anesthetist (CRNA)?
A CRNA is an advanced practice nurse who specializes in anesthesia care. They are responsible for administering anesthesia, monitoring patients during surgery, and providing pain management. CRNAs work in various settings, including hospitals, surgery centers, and pain management clinics, ensuring patient safety and comfort throughout the perioperative process.
2. What are the different types of anesthesia?
- General Anesthesia: Induces a state of unconsciousness and is used for major surgeries.
- Regional Anesthesia: Blocks sensation in a specific area of the body, such as an epidural.
- Local Anesthesia: Numbs a small, localized area for minor procedures.
Understanding these types helps CRNAs select the appropriate method based on the patient’s needs and the surgical procedure.
3. What is the significance of the ASA physical status classification?
The ASA (American Society of Anesthesiologists) physical status classification system helps assess a patient’s pre-anesthesia health status. It ranges from ASA I (healthy) to ASA VI (declared brain-dead). This classification aids CRNAs in evaluating risk factors and planning anesthesia care accordingly, ensuring patient safety during procedures.
Build your resume in just 5 minutes with AI.
4. Can you explain the pharmacokinetics of anesthetic agents?
Pharmacokinetics refers to how the body absorbs, distributes, metabolizes, and excretes drugs. Key factors include:
- Absorption: How quickly a drug enters the bloodstream.
- Distribution: How the drug disperses throughout the body.
- Metabolism: How the body chemically alters the drug.
- Excretion: How the drug is eliminated from the body.
Understanding these processes is crucial for CRNAs to manage anesthesia effectively and tailor drug dosages for individual patients.
5. What are some common complications of anesthesia?
- Respiratory Depression: Reduced breathing rate can occur with certain anesthetics.
- Allergic Reactions: Patients may have adverse reactions to anesthetic agents.
- Nerve Damage: Regional anesthesia can sometimes lead to temporary or permanent nerve injury.
CRNAs must be prepared to recognize and manage these complications to ensure patient safety during anesthesia care.
6. How do you assess a patient’s airway?
Airway assessment involves evaluating the patient’s anatomy and any potential difficulties in intubation. Key components include:
- History: Previous surgeries or breathing problems.
- Physical Exam: Observing the mouth opening, neck mobility, and jaw structure.
- Mallampati Classification: Classifies airway visibility to predict intubation difficulty.
This assessment is critical for planning safe anesthesia management.
7. What is the purpose of preoperative assessment?
The preoperative assessment is vital for identifying patient-specific risks and optimizing care. It includes reviewing medical history, conducting physical exams, and discussing anesthesia plans with the patient. This process helps minimize complications, ensures informed consent, and allows for the customization of anesthesia techniques based on individual needs.
8. Describe the process of induction in anesthesia.
Induction is the process of transitioning a patient from consciousness to unconsciousness for surgery. It typically involves the following steps:
- Pre-oxygenation: Providing oxygen to the patient before anesthesia.
- Administering Induction Agents: Using intravenous or inhalational agents to induce anesthesia.
- Intubation: Inserting an endotracheal tube to secure the airway.
This process ensures a smooth start to surgery while maintaining patient safety.
9. What is the role of monitoring during anesthesia?
Monitoring during anesthesia is essential for ensuring patient safety and managing vital signs effectively. Key parameters monitored include:
- Heart Rate: To detect arrhythmias or distress.
- Blood Pressure: To assess hemodynamic stability.
- Oxygen Saturation: To ensure adequate oxygenation throughout the procedure.
Continuous monitoring allows CRNAs to respond quickly to any changes during anesthesia.
10. What are the effects of anesthetic agents on the cardiovascular system?
Anesthetic agents can have various effects on cardiovascular function, including:
- Hypotension: Many anesthetics can lower blood pressure.
- Increased Heart Rate: Certain agents may cause tachycardia.
- Myocardial Depression: Some agents can reduce heart contractility.
Understanding these effects is crucial for managing patients with existing cardiovascular conditions.
11. What is the recovery process after anesthesia?
The recovery process involves closely monitoring patients as they regain consciousness and vital functions post-anesthesia. Key aspects include:
- Observation: Monitoring vital signs, level of consciousness, and pain management.
- Nausea Management: Administering antiemetics if necessary.
- Assessment of Airway: Ensuring the patient can breathe independently.
A smooth recovery is essential for patient satisfaction and safety.
12. How do CRNAs manage pain in patients?
CRNAs manage pain through various strategies, including:
- Preemptive Analgesia: Administering analgesics before surgery to minimize postoperative pain.
- Multimodal Analgesia: Combining different medications (e.g., opioids, NSAIDs) to enhance pain relief.
- Regional Anesthesia: Using techniques like nerve blocks to provide localized pain control.
Effective pain management improves patient outcomes and satisfaction.
13. What is the importance of informed consent in anesthesia?
Informed consent is a critical aspect of anesthesia practice, ensuring that patients understand the risks, benefits, and alternatives to anesthesia. It promotes patient autonomy and trust in the healthcare system. CRNAs must provide clear explanations, answer questions, and ensure that patients are comfortable with the planned anesthesia approach before proceeding.
14. Describe an adverse reaction to anesthesia and its management.
Anaphylaxis is a severe allergic reaction that can occur with anesthetic agents. Symptoms may include difficulty breathing, swelling, and low blood pressure. Management involves:
- Immediate Discontinuation: Stop administering the offending agent.
- Administration of Epinephrine: Use epinephrine to counteract severe allergic reactions.
- Supportive Care: Provide oxygen and intravenous fluids as needed.
Timely recognition and management are crucial for patient safety in such situations.
15. What is the role of CRNAs in emergency situations?
In emergency situations, CRNAs play a vital role in providing rapid anesthesia care and airway management. They are trained to assess and stabilize patients, administer emergency medications, and perform life-saving procedures such as intubation. Their ability to act swiftly and efficiently in high-pressure environments is essential for positive patient outcomes.
These questions are tailored for freshers entering the Certified Registered Nurse Anesthetist (CRNA) field and cover fundamental concepts they should master.
16. What is the role of a CRNA in a healthcare setting?
A Certified Registered Nurse Anesthetist (CRNA) is an advanced practice nurse who specializes in anesthesia care. They play a critical role in the management of anesthesia for surgical procedures, ensuring patient safety and comfort. CRNAs perform pre-anesthesia assessments, administer anesthesia, monitor patients during procedures, and manage post-anesthesia recovery. Their expertise is essential in both surgical and non-surgical settings, and they often collaborate with surgeons and other healthcare professionals to provide comprehensive care.
17. What are the different types of anesthesia that a CRNA may administer?
- General Anesthesia: This type induces a state of unconsciousness and is typically used for major surgeries.
- Regional Anesthesia: This involves blocking sensation in a specific area, such as an epidural for childbirth.
- Local Anesthesia: This numbs a small area and is often used for minor procedures.
- Monitored Anesthesia Care (MAC): This is a combination of sedation and local anesthesia, used for outpatient procedures.
Each type of anesthesia has its indications, contraindications, and monitoring requirements, making it crucial for CRNAs to have a deep understanding of their applications.
18. Describe the importance of pre-anesthetic assessment.
The pre-anesthetic assessment is a critical component of anesthesia care. During this process, a CRNA evaluates the patient’s medical history, current medications, allergies, and previous anesthesia experiences. This assessment helps identify any potential risks and contraindications for anesthesia, allowing the CRNA to develop an individualized anesthesia plan. Effective communication during this stage also helps to alleviate patient anxiety and ensure informed consent for the anesthesia procedure.
19. What are some common complications associated with anesthesia?
- Hypotension: A drop in blood pressure that can lead to inadequate organ perfusion.
- Nausea and Vomiting: Common side effects that can occur post-anesthesia.
- Airway Obstruction: A potential risk during and after anesthesia, especially in patients with specific anatomical concerns.
- Allergic Reactions: Patients may have adverse reactions to anesthetic agents.
Understanding these complications allows CRNAs to anticipate issues and implement strategies to mitigate risks during anesthesia administration.
20. How do CRNAs monitor a patient during anesthesia?
CRNAs utilize various monitoring techniques to ensure patient safety during anesthesia. They continuously assess vital signs such as heart rate, blood pressure, oxygen saturation, and respiratory rate. Additionally, they may use advanced monitoring tools like capnography to measure exhaled carbon dioxide levels and electrocardiography (ECG) to monitor heart function. By closely observing these parameters, CRNAs can quickly identify any changes and respond appropriately to maintain patient stability throughout the procedure.
21. What is the significance of pain management in anesthesia?
Pain management is a crucial aspect of anesthesia care. Effective pain control can significantly enhance patient outcomes, reduce stress, and improve recovery times. CRNAs use multimodal analgesia, which involves combining different medications and techniques to achieve optimal pain relief while minimizing side effects. This approach not only helps manage pain during surgery but also contributes to better post-operative recovery and overall patient satisfaction.
22. Explain the concept of patient safety in anesthesia practice.
Patient safety is paramount in anesthesia practice. CRNAs are trained to identify and mitigate risks associated with anesthesia administration. This includes rigorous monitoring of patients, adherence to safety protocols, and effective communication with the surgical team. CRNAs also perform thorough assessments and prepare for emergencies, ensuring they have the necessary equipment and medications readily available. By prioritizing safety, CRNAs help prevent adverse events and promote positive surgical outcomes.
CRNA Intermediate Interview Questions
In preparing for CRNA interviews, candidates should focus on intermediate-level concepts that demonstrate their clinical knowledge, critical thinking, and problem-solving abilities. Key topics include pharmacology, anesthesia techniques, and patient assessment, which are essential for providing safe and effective anesthesia care.
23. What are the primary classes of anesthetic agents used in practice?
The primary classes of anesthetic agents include:
- Inhalational Agents: Such as sevoflurane and isoflurane, used for maintenance of general anesthesia.
- Intravenous Agents: Such as propofol and thiopental, primarily used for induction of anesthesia.
- Opioids: Such as fentanyl and morphine, utilized for pain management during and after surgery.
- Local Anesthetics: Such as lidocaine and bupivacaine, used for regional anesthesia techniques.
Understanding these classes and their pharmacokinetics is crucial for effective anesthesia management.
24. Describe the mechanisms of action for local anesthetics.
Local anesthetics work by blocking sodium channels in neuronal cell membranes, preventing the propagation of action potentials. This results in a reversible loss of sensation in a specific area. The onset and duration of action depend on the drug’s lipid solubility, pKa, and protein binding capacity. The use of adjuncts like epinephrine can prolong the effects by causing vasoconstriction.
25. What factors influence the pharmacokinetics of anesthetic drugs?
- Solubility: Lipid solubility affects the potency and duration of anesthetic agents.
- Protein Binding: Higher protein binding can prolong the drug’s effect.
- Volume of Distribution: Affects how the drug is distributed in body compartments.
- Metabolism: The liver’s ability to metabolize drugs influences their duration of action.
- Excretion: Renal function is crucial for the elimination of many anesthetic agents.
Understanding these factors helps in tailoring anesthesia plans to individual patient needs.
26. How do you assess a patient’s airway before anesthesia?
Airway assessment involves several key components:
- Visual Inspection: Checking for facial anomalies, obesity, or neck circumference.
- Thyromental Distance: Measuring the distance from the thyroid notch to the mentum; a shorter distance indicates potential difficulty.
- Mallampati Classification: Evaluating the view of the oropharynx to anticipate intubation challenges.
- Neck Mobility: Assessing the range of motion to predict potential difficulties in positioning.
Thorough assessment ensures preparedness for potential airway complications.
27. Explain the significance of the ASA physical status classification.
The ASA (American Society of Anesthesiologists) physical status classification is a system used to assess a patient’s preoperative health. It ranges from ASA I (healthy) to ASA VI (declared brain dead). This classification helps anesthetists evaluate the risk of anesthesia and surgery, guiding preoperative planning and intraoperative management to improve patient safety and outcomes.
28. What are the indications and contraindications for regional anesthesia?
- Indications: Major surgeries on the lower abdomen, pelvis, and lower extremities; postoperative analgesia; patients with respiratory issues who cannot tolerate general anesthesia.
- Contraindications: Patient refusal; infection at the injection site; coagulopathy; significant anatomical abnormalities; and allergy to local anesthetics.
Knowing these factors helps to optimize patient safety and comfort during procedures.
29. Discuss the potential complications of general anesthesia.
- Respiratory Complications: Such as airway obstruction, hypoventilation, or aspiration.
- Cardiovascular Issues: Including hypotension, arrhythmias, or myocardial infarction.
- Neurological Effects: Potential awareness during anesthesia or postoperative cognitive dysfunction.
- Malignant Hyperthermia: A rare but life-threatening condition triggered by certain anesthetic agents.
Awareness and preparation for these complications are critical for safe anesthesia practice.
30. What is the role of neuromuscular blocking agents in anesthesia?
Neuromuscular blocking agents (NMBAs) are used to facilitate intubation and provide muscle relaxation during surgery. They work by blocking the transmission of nerve impulses at the neuromuscular junction. It is essential to monitor the depth of neuromuscular block to avoid complications such as residual paralysis, which can lead to respiratory failure postoperatively.
31. How do you manage a patient experiencing hypotension during anesthesia?
- Assess the cause: Check for volume status, depth of anesthesia, and possible drug effects.
- Fluid Resuscitation: Administer IV fluids to restore circulating volume.
- Medications: Use vasopressors like ephedrine or phenylephrine if fluid resuscitation is insufficient.
- Positioning: Consider placing the patient in a Trendelenburg position to improve venous return.
Prompt recognition and management of hypotension are crucial to maintaining hemodynamic stability.
32. What are the considerations for anesthesia in geriatric patients?
- Pharmacokinetics: Altered metabolism and clearance necessitate dose adjustments.
- Comorbidities: Higher prevalence of cardiovascular and respiratory diseases requires careful assessment.
- Cognitive Function: Increased risk of postoperative delirium; preoperative cognitive assessment is recommended.
- Polypharmacy: Interactions with existing medications must be carefully managed.
Tailoring anesthetic techniques and monitoring strategies to the geriatric population is essential for optimal outcomes.
33. Describe the process of anesthesia induction.
Anesthesia induction involves several steps:
- Pre-oxygenation: Providing supplemental oxygen to increase blood oxygen levels.
- Administration of Induction Agent: Administering agents like propofol or thiopental via IV.
- Airway Management: Securing the airway through intubation or use of a supraglottic device.
- Monitoring: Continuously assessing vital signs and responsiveness throughout the process.
Effective induction is crucial for patient safety and sets the stage for a smooth surgical procedure.
34. What are the common anesthetic monitoring techniques?
- Electrocardiography (ECG): Monitoring heart rhythm and rate.
- Pulse Oximetry: Assessing oxygen saturation levels.
- Capnography: Measuring exhaled carbon dioxide to evaluate ventilation.
- Blood Pressure Monitoring: Continuous assessment of hemodynamics.
- Temperature Monitoring: Ensuring normothermia during procedures.
These monitoring techniques are vital for early detection of complications and ensuring patient safety during anesthesia.
35. Explain the concept of balanced anesthesia.
Balanced anesthesia refers to the use of multiple agents to achieve optimal anesthesia with minimal side effects. This typically involves combining an inhalational agent, an opioid, and a muscle relaxant, allowing for lower doses of each agent. This approach enhances analgesia, reduces the risk of adverse effects, and allows for quicker recovery. It provides a tailored anesthetic experience based on the surgical procedure and patient characteristics.
Here are some intermediate-level interview questions for Certified Registered Nurse Anesthetists (CRNAs). These questions cover practical applications and important considerations in the field.
38. What are the primary responsibilities of a CRNA during a surgical procedure?
The primary responsibilities of a CRNA during a surgical procedure include conducting pre-anesthesia assessments, developing and implementing anesthesia care plans, administering anesthesia medications, monitoring the patient’s vital signs and anesthesia levels during the procedure, and ensuring patient safety throughout the surgery. Additionally, CRNAs are also responsible for responding to any complications or emergencies that arise during the anesthetic process.
39. How do you determine the appropriate anesthesia plan for a patient?
Determining the appropriate anesthesia plan involves several critical considerations:
- Patient medical history: Review of any comorbidities, allergies, and previous anesthesia experiences.
- Type of surgery: Understanding the surgical procedure’s complexity and duration to select suitable anesthesia techniques.
- Patient preferences: Discussing with the patient their concerns and preferences regarding anesthesia.
- Risk assessment: Evaluating the patient’s risk factors to tailor the anesthesia plan accordingly.
This comprehensive approach ensures that the anesthesia plan is safe and effective for each individual patient.
40. Describe a time when you had to manage a difficult airway. What steps did you take?
In managing a difficult airway, I first assessed the patient’s anatomy and any contributing factors that could complicate intubation. I utilized the following steps:
- Preparation: Ensured all necessary equipment was available, including various sizes of endotracheal tubes and airway adjuncts.
- Positioning: Optimized the patient’s position to improve airway access.
- Technique: Used a video laryngoscope for better visualization, and if needed, I performed a bougie-assisted intubation.
- Backup plans: Prepared for alternative airway management strategies, such as using a laryngeal mask airway or rescue devices.
This systematic approach minimizes risk and enhances patient safety during challenging situations.
41. What are some common complications associated with anesthesia, and how can they be mitigated?
Common complications associated with anesthesia include:
- Hypotension: Can be mitigated by fluid resuscitation and careful monitoring of vital signs.
- Respiratory depression: Managed through careful titration of anesthetic agents and continuous monitoring of oxygen saturation.
- Nausea and vomiting: Preventive medications can be administered preoperatively to reduce the risk.
- Allergic reactions: Thorough preoperative assessments can help identify patients at risk.
By anticipating these complications and implementing preventive strategies, CRNAs can significantly improve patient outcomes.
42. Explain the pharmacokinetics and pharmacodynamics of a commonly used anesthetic agent.
Let’s consider Propofol as an example:
- Pharmacokinetics: Propofol is rapidly distributed and metabolized in the liver. It has a quick onset of action, usually within 30 seconds, and a short half-life, allowing for rapid recovery.
- Pharmacodynamics: It acts as a GABA receptor agonist, enhancing inhibitory neurotransmission, which results in sedation and anesthesia.
The rapid onset and short duration make Propofol a versatile choice for both induction and maintenance of anesthesia.
43. How do you assess the effectiveness of anesthesia during surgery?
Assessing the effectiveness of anesthesia involves monitoring several key indicators:
- Vital signs: Continuous monitoring of heart rate, blood pressure, and oxygen saturation helps gauge the patient’s physiological response.
- Depth of anesthesia: Evaluating the patient’s responsiveness to stimuli, such as movement or changes in vital signs, can indicate the level of anesthesia.
- Neuromuscular function: Using a peripheral nerve stimulator can help assess the depth of neuromuscular blockade if applicable.
These assessments ensure that the anesthesia remains effective throughout the surgical procedure, adjusting as necessary.
44. What role does teamwork play in the anesthesia care team, and how do you facilitate effective communication?
Teamwork is crucial in the anesthesia care team, as it enhances patient safety and improves outcomes. To facilitate effective communication, I prioritize the following:
- Preoperative briefing: Conducting a thorough briefing with the surgical team to discuss the anesthesia plan and any concerns.
- Clear communication: Using standardized communication tools, such as SBAR (Situation, Background, Assessment, Recommendation), to ensure information is conveyed effectively.
- Encouragement: Fostering an environment where team members feel comfortable voicing concerns or suggestions.
By focusing on these aspects, I help create a collaborative atmosphere that is essential for successful anesthesia management.
CRNA Interview Questions for Experienced
This section provides advanced CRNA interview questions tailored for experienced professionals. These questions delve into critical topics such as anesthesia techniques, patient safety, pharmacology, leadership in clinical settings, and complex case management, ensuring candidates demonstrate their expertise and strategic thinking in high-pressure environments.
45. What are the key considerations when designing an anesthesia plan for a patient with multiple comorbidities?
When designing an anesthesia plan for a patient with multiple comorbidities, key considerations include:
- Comorbidity assessment: Understanding how each condition affects anesthesia management.
- Medication interactions: Evaluating current medications to prevent adverse effects.
- Risk stratification: Determining the patient’s overall risk for complications during and after surgery.
- Monitoring requirements: Tailoring intraoperative monitoring to the patient’s specific needs.
- Postoperative care: Planning for enhanced recovery protocols based on comorbidities.
A thorough preoperative evaluation is crucial to ensure patient safety and optimize outcomes.
46. How does the choice of anesthetic agents impact patient outcomes?
The choice of anesthetic agents can significantly impact patient outcomes based on factors such as:
- Pharmacokinetics: Different agents have varying onset and duration of action which can affect recovery times.
- Patient-specific factors: Individual patient responses to anesthesia can influence efficacy and safety.
- Procedure type: Certain surgeries may require specific agents to optimize patient stability and pain management.
- Side effects: Each agent has a unique profile of potential side effects, which can affect postoperative recovery.
Selecting the appropriate anesthetic requires a balance between effectiveness and safety tailored to the patient’s needs.
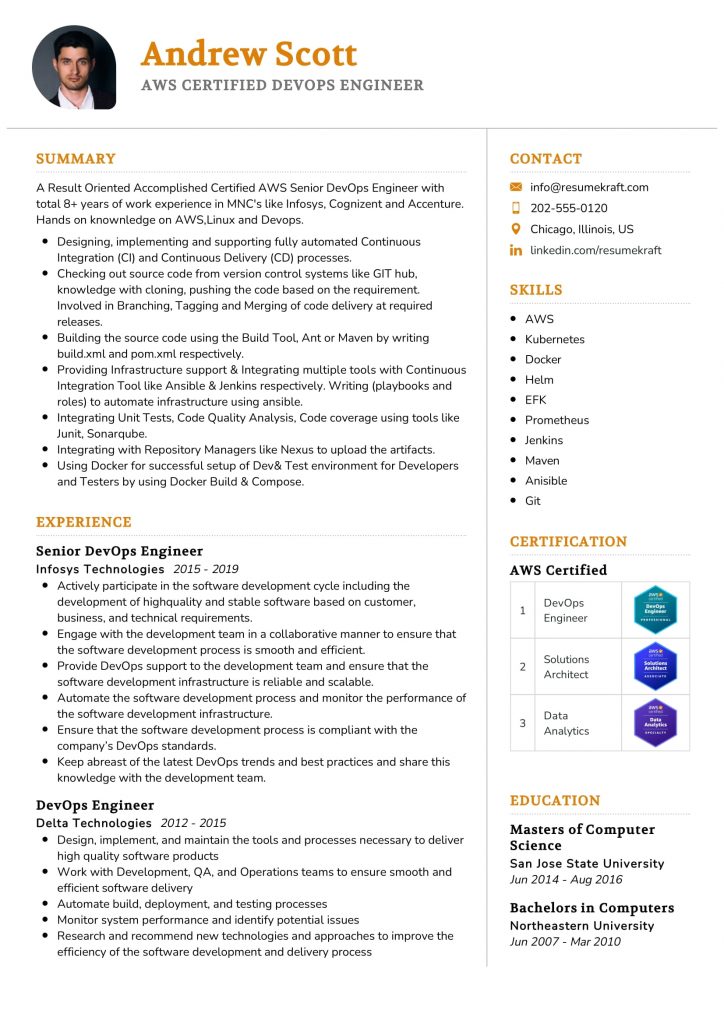
Build your resume in 5 minutes
Our resume builder is easy to use and will help you create a resume that is ATS-friendly and will stand out from the crowd.
47. Describe a challenging case you managed and the leadership skills you employed.
In a challenging case involving a patient with a severe allergy to multiple anesthetic agents, I had to demonstrate strong leadership and critical thinking. I coordinated a multidisciplinary team to assess alternative agents, ensuring thorough communication with surgical staff and the patient. I implemented an allergy management protocol and monitored the patient closely. This experience highlighted the importance of teamwork, adaptability, and clear communication in crisis situations.
48. What are the principles of the ASA physical status classification system?
The ASA physical status classification system is used to assess a patient’s pre-anesthesia medical fitness. The principles include:
- Class I: Healthy, no systemic disease.
- Class II: Mild systemic disease.
- Class III: Severe systemic disease.
- Class IV: Severe systemic disease that is a constant threat to life.
- Class V: Moribund patient who is not expected to survive without surgery.
- Class VI: Declared brain-dead patient whose organs are being removed for donor purposes.
- Class ASA PS: Unassigned, used for patients with multiple issues or unknown status.
Understanding these classifications aids in risk assessment and management during anesthesia.
49. How do you ensure optimal patient safety in the perioperative setting?
To ensure optimal patient safety in the perioperative setting, I focus on several strategies:
- Thorough preoperative assessments: Evaluating patient history and comorbidities.
- Standardized protocols: Implementing checklists and protocols to minimize errors.
- Effective communication: Encouraging open dialogue within the surgical team to address concerns.
- Continuous monitoring: Utilizing advanced monitoring technologies during procedures.
- Postoperative follow-up: Ensuring proper care and addressing complications promptly.
These measures create a comprehensive safety net that enhances patient outcomes.
50. Discuss the importance of fluid management during anesthesia.
Fluid management during anesthesia is crucial for maintaining hemodynamic stability. Key considerations include:
- Preoperative assessment: Evaluating volume status and fluid needs based on the patient’s condition.
- Type of procedure: Understanding how surgery type impacts fluid requirements.
- Monitoring: Continuously assessing fluid balance and adjusting administration as needed.
- Electrolyte balance: Ensuring that electrolytes remain within normal ranges to prevent complications.
Proper fluid management reduces the risk of intraoperative complications and aids in patient recovery.
51. What role does mentorship play in CRNA practice?
Mentorship plays a vital role in CRNA practice by fostering professional development and enhancing clinical skills. Key aspects include:
- Knowledge transfer: Experienced CRNAs can share insights and best practices.
- Support: Mentors provide emotional and professional support, guiding mentees through challenges.
- Career advancement: Mentorship can open doors to opportunities in leadership and specialized practice.
- Networking: Connecting mentees with professional organizations and resources.
Effective mentorship fosters a culture of learning and excellence in anesthesia practice.
52. Explain the concept of anesthesia depth and its significance.
Anesthesia depth refers to the level of unconsciousness and analgesia achieved during anesthesia. Its significance includes:
- Patient safety: Ensuring that patients are adequately anesthetized to prevent awareness during procedures.
- Procedure requirements: Matching anesthesia depth to the surgical procedure type to optimize outcomes.
- Recovery: A deeper anesthesia may prolong recovery times, impacting patient turnover in facilities.
Monitoring anesthesia depth is essential for tailoring care to individual patient needs and surgical demands.
53. How do you approach a case involving a patient with a history of substance abuse?
Approaching a case involving a patient with a history of substance abuse requires sensitivity and careful planning. Key steps include:
- Thorough assessment: Evaluating the extent of substance use and its impact on health.
- Collaborative care: Engaging a multidisciplinary team to manage the patient’s needs.
- Tailored anesthetic plan: Selecting agents and dosages that minimize the risk of complications.
- Postoperative support: Providing resources for addiction treatment and monitoring recovery.
This approach promotes safety while addressing the unique challenges presented by substance abuse.
54. What are the ethical considerations in CRNA practice?
Ethical considerations in CRNA practice are paramount, including:
- Informed consent: Ensuring patients understand the risks and benefits of anesthesia.
- Patient autonomy: Respecting patient choices while providing professional recommendations.
- Confidentiality: Maintaining patient privacy and protecting sensitive information.
- Equity in care: Providing fair treatment regardless of background or circumstances.
Adhering to ethical principles fosters trust and enhances the quality of care delivered to patients.
55. Discuss the impact of technology on anesthesia practice.
Technology has significantly impacted anesthesia practice in various ways:
- Advanced monitoring: Technologies such as bispectral index (BIS) monitors enhance patient safety by providing real-time data on anesthesia depth.
- Simulation training: Virtual simulations allow CRNAs to practice skills and decision-making in a risk-free environment.
- Telemedicine: Remote consultations enable CRNAs to provide preoperative assessments and follow-ups efficiently.
- Electronic health records: Streamlining documentation and improving communication among healthcare providers.
These advancements improve patient care, enhance safety, and optimize workflow in anesthesia practice.
56. How do you handle complications during anesthesia?
Handling complications during anesthesia involves a systematic approach:
- Immediate assessment: Quickly evaluating the situation to identify the nature and severity of the complication.
- Communication: Informing the surgical team and discussing the necessary interventions.
- Implementation of protocols: Utilizing established protocols to manage specific complications, such as airway emergencies or hemodynamic instability.
- Post-event debriefing: Analyzing the incident afterward to improve future responses and patient safety.
Effective management of complications requires both technical skill and strong teamwork.
These questions are tailored for experienced Certified Registered Nurse Anesthetists (CRNAs) and focus on advanced concepts in anesthesia practice, patient care, and leadership within the healthcare environment.
60. How do you ensure patient safety during anesthesia administration?
Ensuring patient safety during anesthesia involves several critical steps: conducting thorough preoperative assessments, verifying patient identity and surgical site, and continuously monitoring vital signs throughout the procedure. Additionally, employing the ASA (American Society of Anesthesiologists) guidelines helps standardize practices. It is also essential to stay updated with the latest safety protocols and engage in team communication to address any concerns promptly. Regularly participating in simulation training enhances preparedness for emergencies, ultimately safeguarding patient outcomes.
61. Can you explain the importance of pharmacokinetics and pharmacodynamics in anesthesia?
- Pharmacokinetics: This refers to how the body absorbs, distributes, metabolizes, and excretes anesthetic agents. Understanding these processes helps CRNAs determine the appropriate dosages and timing for administration.
- Pharmacodynamics: This involves how anesthetic drugs affect the body, including their mechanisms of action and effects on different organ systems. Knowledge of pharmacodynamics is crucial for predicting patient responses and managing potential side effects.
In summary, a solid grasp of both pharmacokinetics and pharmacodynamics is essential for safe and effective anesthesia management, enabling CRNAs to tailor anesthetic plans to individual patient needs.
62. Describe a design pattern you have implemented in your practice as a CRNA.
One effective design pattern in anesthesia practice is the “Observer” pattern, particularly during multi-disciplinary team communication. In this context, the CRNA acts as an observer, closely monitoring the patient’s status while updating the surgical team and other healthcare providers in real-time. This allows for prompt responses to any changes in the patient’s condition. Implementing structured handoff protocols ensures that all team members are informed about critical patient information, enhancing collaboration and patient safety.
How to Prepare for Your CRNA Interview
Preparing for a Certified Registered Nurse Anesthetist (CRNA) interview requires a strategic approach. Focus on understanding the role, showcasing your clinical experience, and demonstrating your commitment to patient care. Here are some effective tips to help you stand out during the interview process.
- Understand the Role: Research the responsibilities of a CRNA, including anesthesia administration and patient management. Familiarize yourself with different types of anesthesia and their applications. This knowledge will demonstrate your commitment and readiness for the role during the interview.
- Review Clinical Experiences: Reflect on your clinical experiences related to anesthesia. Be prepared to discuss specific cases, challenges faced, and how you handled them. Highlighting your hands-on experience will show your competence and confidence in the field.
- Practice Common Interview Questions: Prepare for frequently asked interview questions, such as your motivation for becoming a CRNA and your approach to handling difficult situations. Practicing these responses will help you articulate your thoughts clearly and confidently during the interview.
- Know the Program: Research the CRNA program you are interviewing for. Understand their values, mission, and curriculum. This knowledge will allow you to tailor your responses and show your genuine interest in their specific program.
- Prepare Questions to Ask: Develop insightful questions to ask the interviewers about the program, faculty, and clinical experiences. This not only shows your interest but also helps you gather important information to make an informed decision if offered a position.
- Highlight Teamwork and Collaboration: Be ready to discuss your experiences working in a team-based environment. Emphasize your ability to collaborate with other healthcare professionals, as teamwork is crucial in anesthesia practice for patient safety and effective care.
- Showcase Professionalism: Dress appropriately for the interview and demonstrate professionalism in your communication. Punctuality, body language, and respectful interaction can leave a lasting impression, reflecting your dedication to the nursing profession and the CRNA role.
Common CRNA Interview Mistakes to Avoid
Preparing for a Certified Registered Nurse Anesthetist (CRNA) interview requires vigilance, as certain common mistakes can hinder your chances. Understanding these pitfalls can help you present your best self and increase your chances of success.
- Inadequate Research: Failing to research the institution or specific anesthesia practices can make you seem uninterested. Knowledge about the facility’s values, mission, and practices demonstrates genuine interest and preparedness.
- Poor Communication Skills: Effective communication is crucial in healthcare. Failing to articulate your thoughts clearly or using overly technical jargon can confuse interviewers and hinder your ability to convey your passion for anesthesia.
- Neglecting Behavioral Questions: Many interviews include behavioral questions that assess your past experiences. Not preparing for these can lead to vague or irrelevant answers, making it difficult to showcase your problem-solving and critical-thinking skills.
- Overemphasizing Technical Skills: While technical expertise is essential, focusing solely on it can neglect the importance of soft skills like teamwork, empathy, and patient communication, which are vital in anesthesia practice.
- Not Asking Questions: Failing to ask thoughtful questions can signal a lack of curiosity or engagement. Prepare insightful questions to demonstrate your interest in the role and the institution.
- Inadequate Self-Presentation: Not paying attention to your appearance or body language can create a negative impression. Dress professionally and maintain good posture to convey confidence and professionalism.
- Being Unprepared for Scenario Questions: Interviewers often present clinical scenarios to assess decision-making skills. Not practicing these scenarios can lead to unstructured or incomplete responses, failing to highlight your critical thinking.
- Ignoring Follow-Up Etiquette: Neglecting to send a thank-you note post-interview can be seen as unprofessional. A thoughtful follow-up reinforces your interest and leaves a positive impression on the interviewers.
Key Takeaways for CRNA Interview Success
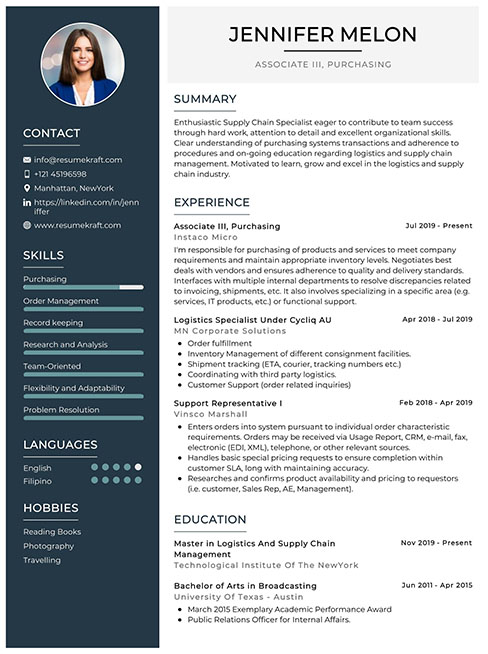
- Prepare a polished resume using AI resume builder tools to highlight your strengths. Ensure it aligns with industry standards and showcases your relevant experience effectively.
- Utilize well-structured resume templates to organize your information clearly. A clean format helps your qualifications stand out, making it easier for interviewers to assess your suitability.
- Include resume examples that demonstrate your clinical experience and academic achievements. Tailor these examples to reflect the specific requirements of the CRNA role you are applying for.
- Craft compelling cover letters that articulate your passion for anesthesia and your career goals. This personal touch can make a significant difference in your application’s impact.
- Engage in mock interview practice to refine your responses and build confidence. This preparation will help you articulate your thoughts clearly and effectively during the actual interview.
Frequently Asked Questions
1. How long does a typical CRNA interview last?
A typical CRNA interview can last anywhere from 30 minutes to 2 hours, depending on the institution and the structure of the interview process. Expect a combination of behavioral and clinical questions, as well as discussions about your experience and motivation for pursuing the CRNA role. Being well-prepared to articulate your clinical experiences and understanding of anesthesia practice will help you make the most of the time allocated.
2. What should I wear to a CRNA interview?
For a CRNA interview, it’s essential to dress professionally to create a good first impression. A tailored suit in neutral colors is a safe choice for both men and women. Women may opt for a suit with a blouse, while men should consider a dress shirt and tie. Ensure your attire is clean, pressed, and appropriate for a medical setting. Also, pay attention to grooming; a polished appearance reflects your professionalism and seriousness about the role.
3. How many rounds of interviews are typical for a CRNA position?
Typically, there are one to three rounds of interviews for a CRNA position. The first round may involve a panel interview with faculty or hiring managers, focusing on your clinical skills and experiences. Subsequent rounds might include a more in-depth discussion of your qualifications or situational judgment assessments. Some programs may also require a practical component or simulation assessment. Being prepared for varied formats will help you navigate the interview process successfully.
4. Should I send a thank-you note after my CRNA interview?
Yes, sending a thank-you note after your CRNA interview is highly recommended. It demonstrates professionalism and appreciation for the opportunity to interview. In your note, express gratitude for the interviewers’ time, reiterate your interest in the position, and briefly highlight how your skills align with the program’s goals. A well-crafted thank-you note can leave a positive impression and reinforce your enthusiasm for the role.