Preparing for a Medicine and Health Services Manager interview is a critical step in securing a role that blends healthcare expertise with management skills. This unique position involves overseeing the delivery of healthcare services, managing staff, and ensuring compliance with regulations, making it essential for candidates to demonstrate both clinical knowledge and leadership abilities. Proper interview preparation not only boosts confidence but also equips candidates with the tools to effectively convey their qualifications and fit for the role. This comprehensive guide will cover common interview questions, key skills to highlight, and strategies for showcasing your experience, ensuring you stand out in this competitive field.
- What to Expect in a Medicine and Health Services Manager Interview
- Medicine and Health Services Manager Interview Questions For Freshers
- Medicine and Health Services Manager Intermediate Interview Questions
- Medicine and Health Services Manager Interview Questions for Experienced
- How to Prepare for Your Medicine and Health Services Manager Interview
What to Expect in a Medicine and Health Services Manager Interview
In a Medicine and Health Services Manager interview, candidates can expect a mix of behavioral and situational questions aimed at assessing their leadership, communication, and problem-solving skills. Interviews may be conducted by a panel that includes healthcare executives, human resources representatives, and current health services managers. The process typically begins with an introductory conversation, followed by questions about past experiences, and may include case studies or role-playing scenarios to evaluate decision-making abilities. Candidates should also be prepared to discuss healthcare regulations and their impact on management practices.
Medicine and Health Services Manager Interview Questions For Freshers
This set of interview questions is tailored for freshers aspiring to become Medicine and Health Services Managers. Candidates should master fundamental concepts such as healthcare operations, regulatory compliance, financial management, and patient care quality to excel in their interviews.
1. What are the primary responsibilities of a Medicine and Health Services Manager?
A Medicine and Health Services Manager is responsible for overseeing the operations of healthcare facilities. Their primary duties include managing staff, ensuring compliance with healthcare regulations, budgeting, and improving the quality of patient care. They also coordinate between departments to enhance efficiency and patient satisfaction while managing resources effectively.
2. How do you ensure compliance with healthcare regulations?
Ensuring compliance with healthcare regulations involves several key steps:
- Regular Training: Conduct ongoing training for staff on relevant laws and policies.
- Audits: Perform audits to identify areas of non-compliance and address them promptly.
- Documentation: Maintain accurate records and documentation to demonstrate compliance during inspections.
By actively monitoring compliance and staying updated on regulations, managers can mitigate risks and avoid penalties.
3. Describe your approach to managing a healthcare budget.
Managing a healthcare budget requires a systematic approach, including:
- Forecasting: Analyze historical data and trends to predict future expenses and revenues.
- Cost Control: Identify areas where costs can be reduced without compromising patient care.
- Regular Review: Continuously monitor budget performance and adjust as necessary to stay on track.
This proactive management helps ensure the financial health of the organization.
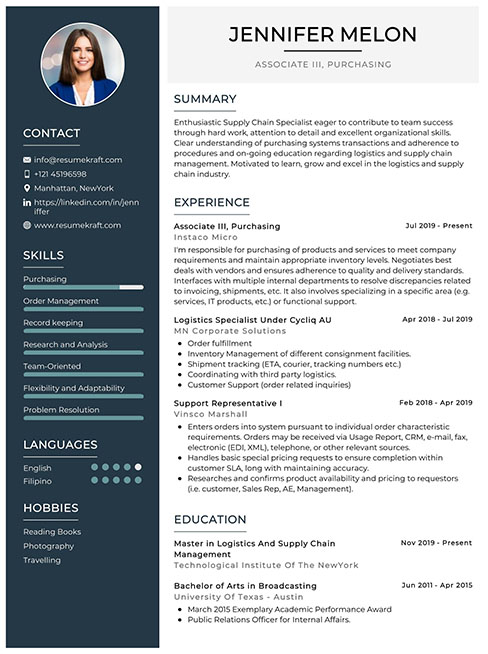
Build your resume in just 5 minutes with AI.
4. What strategies can be used to improve patient care quality?
Improving patient care quality can be achieved through various strategies:
- Feedback Systems: Implementing patient feedback systems to gather insights for improvement.
- Staff Training: Regularly training staff on best practices and new technologies.
- Data Analysis: Utilizing data analytics to identify trends and areas needing enhancement.
These strategies foster a culture of continuous improvement in patient care.
5. How would you handle a conflict between staff members?
Handling staff conflicts requires a calm and structured approach:
- Listen: First, allow each party to express their concerns without interruption.
- Mediate: Facilitate a discussion to help both parties understand each other’s viewpoints.
- Resolution: Guide them toward a mutually agreeable solution and follow up to ensure the issue has been resolved.
This ensures a harmonious work environment and maintains team cohesion.
6. What role does technology play in healthcare management?
Technology plays a crucial role in healthcare management by enhancing efficiency and patient care. Key aspects include:
- Electronic Health Records (EHR): Streamlining patient data management and improving accessibility.
- Telemedicine: Expanding access to care and allowing for remote consultations.
- Data Analytics: Supporting decision-making through insights derived from patient data.
Overall, technology improves operational workflows and patient outcomes.
7. Can you explain the importance of patient confidentiality?
Patient confidentiality is vital for several reasons:
- Trust: It fosters trust between patients and healthcare providers, encouraging open communication.
- Legal Compliance: Adhering to laws such as HIPAA protects patient information and avoids legal consequences.
- Reputation: Maintaining confidentiality enhances the facility’s reputation and patient loyalty.
Ensuring confidentiality is a fundamental ethical obligation in healthcare.
8. What is the significance of staff training in healthcare management?
Staff training is significant for multiple reasons:
- Quality of Care: Trained staff are better equipped to provide high-quality patient care.
- Regulatory Compliance: Ongoing training helps ensure staff are aware of current regulations and standards.
- Employee Satisfaction: Investing in training can boost morale and reduce turnover rates.
Overall, training contributes to a skilled and motivated workforce.
9. How do you measure the effectiveness of healthcare services?
Measuring effectiveness involves utilizing various metrics, such as:
- Patient Satisfaction Surveys: Collecting feedback directly from patients about their experience.
- Health Outcomes: Analyzing patient outcomes and recovery rates to assess service quality.
- Operational Efficiency: Reviewing wait times, readmission rates, and resource utilization.
These metrics provide insights into areas for improvement and ensure quality care delivery.
10. What are the challenges faced in healthcare management?
Healthcare management faces several challenges, including:
- Regulatory Changes: Keeping up with constantly evolving healthcare laws and regulations.
- Resource Allocation: Effectively allocating limited resources while maintaining quality care.
- Staffing Issues: Managing workforce shortages and ensuring adequate staffing levels.
Addressing these challenges requires strategic planning and effective leadership.
11. How do you prioritize tasks in a busy healthcare environment?
Prioritizing tasks involves assessing urgency and impact. Key steps include:
- Assessment: Evaluate tasks based on their importance to patient care and operational efficiency.
- Delegation: Assign tasks to appropriate team members based on their skills and workload.
- Continuous Review: Regularly reassess priorities as situations change in a dynamic environment.
This ensures that critical tasks are completed promptly, enhancing overall service delivery.
12. Describe your experience with healthcare regulations.
While freshers may not have extensive experience, they should be familiar with key regulations like HIPAA, which governs patient privacy, and Medicare/Medicaid regulations for billing. Understanding these frameworks is essential for compliance and operational success. Additionally, familiarity with accreditation standards can help in maintaining facility standards and enhancing patient care.
13. What is your approach to implementing new healthcare policies?
Implementing new healthcare policies requires a systematic approach:
- Communication: Clearly communicate the new policy to all stakeholders, explaining its purpose and benefits.
- Training: Provide staff training to ensure understanding and compliance with the new policy.
- Monitoring: Continuously monitor the policy’s implementation and gather feedback for adjustments.
This structured approach aids in smooth transitions and effective policy adoption.
14. How do you handle budget cuts in a healthcare facility?
Handling budget cuts involves strategic planning and prioritization:
- Identify Essential Services: Determine which services are critical and should be preserved.
- Cost Reduction: Explore options for reducing costs, such as renegotiating contracts or optimizing resource use.
- Stakeholder Communication: Keep open lines of communication with staff and stakeholders to manage expectations and maintain morale.
These strategies can help navigate financial constraints while maintaining quality care.
15. What is the role of patient advocacy in healthcare management?
Patient advocacy is fundamental in healthcare management as it ensures that patients’ needs and rights are prioritized. Key aspects include:
- Empowerment: Advocating for patients empowers them to make informed decisions about their care.
- Quality Improvement: Listening to patient concerns can lead to improvements in service delivery.
- Ethical Obligations: Advocacy aligns with ethical responsibilities to provide equitable care.
Effective patient advocacy fosters a patient-centered approach, enhancing overall healthcare quality.
The following interview questions are tailored for freshers aspiring to enter the field of Medicine and Health Services Management. These questions cover fundamental concepts and basic knowledge relevant to the role.
16. What is the role of a Medicine and Health Services Manager?
A Medicine and Health Services Manager is responsible for overseeing the operational aspects of healthcare facilities. Their role includes managing staff, budgeting, ensuring compliance with regulations, and improving the quality of care provided to patients. They work to streamline processes, implement health policies, and coordinate between departments to enhance efficiency and patient satisfaction.
17. What are some key skills required for a successful career in Health Services Management?
- Leadership: Ability to lead and motivate healthcare teams effectively.
- Communication: Strong verbal and written communication skills for interacting with staff, patients, and stakeholders.
- Analytical Skills: Proficiency in analyzing data to improve healthcare services and operations.
- Financial Acumen: Understanding budgeting and financial management within healthcare settings.
- Problem-Solving: Capacity to identify issues and implement solutions in a timely manner.
These skills are essential for navigating the complexities of healthcare management and ensuring the delivery of quality care.
18. How do healthcare regulations impact health services management?
Healthcare regulations play a critical role in health services management by establishing standards for patient care, safety, and data privacy. Managers must ensure compliance with these regulations to avoid penalties and maintain accreditation. This includes understanding laws such as the Health Insurance Portability and Accountability Act (HIPAA) and the Affordable Care Act (ACA), which shape operational policies and patient interactions.
19. What is the importance of quality improvement in healthcare?
Quality improvement in healthcare is vital for enhancing patient outcomes, reducing errors, and increasing efficiency. It involves systematic efforts to improve processes and services, ensuring that patients receive the best possible care. Methods such as Six Sigma and Lean management are often employed to identify areas for improvement and implement changes that lead to better health outcomes and patient satisfaction.
20. Can you explain the concept of patient-centered care?
Patient-centered care is an approach that prioritizes the needs, preferences, and values of patients in the healthcare process. It emphasizes active collaboration between patients and healthcare providers, ensuring that treatment plans align with the patient’s individual goals. This approach enhances patient satisfaction, promotes adherence to treatment, and often leads to better health outcomes.
21. What technologies are commonly used in health services management?
- Electronic Health Records (EHR): Digitized patient records that improve data accessibility and sharing.
- Telehealth Services: Technology that allows for remote patient consultations, improving access to care.
- Health Information Systems: Tools for managing operational data, scheduling, and billing.
- Data Analytics Software: Programs used to analyze patient data and operational metrics for better decision-making.
These technologies help streamline operations, enhance patient care, and improve overall efficiency in healthcare settings.
22. How does effective budgeting affect health services management?
Effective budgeting is crucial in health services management as it ensures that resources are allocated efficiently. A well-planned budget allows managers to forecast expenses, manage costs, and invest in necessary services and technologies. It also helps in identifying areas of overspending and provides a framework for financial accountability, which is essential for the sustainability of healthcare organizations.
23. What challenges do health services managers face today?
- Regulatory Compliance: Keeping up with changing healthcare laws and regulations can be challenging.
- Resource Allocation: Balancing limited resources while meeting patient needs and organizational goals.
- Technological Adaptation: Implementing and managing new technologies while ensuring staff are trained effectively.
- Patient Satisfaction: Addressing diverse patient needs and expectations within limited time and resources.
These challenges require health services managers to be adaptable, proactive, and skilled in problem-solving to ensure high-quality care and operational efficiency.
Medicine and Health Services Manager Intermediate Interview Questions
As candidates prepare for interviews for the Medicine and Health Services Manager role, they should focus on mid-level concepts such as healthcare regulations, resource management, and operational efficiency. Understanding the complexities of health systems and effective leadership qualities will be crucial for success in this field.
24. What are the key responsibilities of a Medicine and Health Services Manager?
A Medicine and Health Services Manager is responsible for overseeing the operations of a healthcare facility. Key responsibilities include managing staff, ensuring compliance with healthcare regulations, budgeting and financial management, implementing health policies, and improving the quality of care provided to patients. They also coordinate between departments and handle the administrative aspects of healthcare delivery.
25. How do you manage healthcare budgets effectively?
Effective healthcare budget management involves several key practices:
- Assessing current financial performance: Regularly review financial statements to understand revenue and expense trends.
- Setting realistic goals: Establish clear financial goals that align with the organization’s mission and objectives.
- Monitoring expenditures: Implement a system for tracking spending to ensure it remains within budget.
- Identifying cost-saving opportunities: Analyze operations to find areas where costs can be reduced without compromising quality.
By maintaining a clear understanding of financial data and fostering a culture of accountability, managers can ensure the sustainability of healthcare services.
26. What role does technology play in healthcare management?
Technology plays a crucial role in healthcare management by enhancing operational efficiency and improving patient care. Key applications include electronic health records (EHRs) for streamlined patient information access, telemedicine for remote consultations, and data analytics for informed decision-making. Furthermore, technology facilitates better communication among healthcare teams and enhances the overall patient experience.
27. How do you ensure compliance with healthcare regulations?
Ensuring compliance with healthcare regulations involves several essential steps:
- Staying informed: Regularly update knowledge on local, state, and federal healthcare laws and regulations.
- Conducting audits: Perform regular audits of processes and practices to identify any compliance gaps.
- Training staff: Provide ongoing training for employees on compliance policies and procedures.
- Implementing policies: Develop and enforce clear policies that align with regulatory requirements.
By proactively addressing compliance, managers can mitigate risks and enhance the facility’s reputation.
28. Describe a situation where you had to resolve a conflict within your team.
In a past role, I encountered a situation where two department heads disagreed on resource allocation for a project. I facilitated a meeting where each party could present their viewpoints and supporting data. By encouraging open communication and collaboration, we identified a compromise that addressed both departments’ needs while aligning with the organization’s goals. This approach not only resolved the conflict but also fostered a stronger working relationship between departments.
29. What strategies do you employ to improve patient satisfaction?
Improving patient satisfaction requires a multi-faceted approach:
- Gathering feedback: Regularly solicit patient feedback through surveys and focus groups to identify areas for improvement.
- Staff training: Invest in training for staff on customer service and communication skills.
- Streamlining processes: Analyze patient flow and reduce wait times where possible to enhance the patient experience.
- Personalizing care: Encourage staff to build rapport with patients and address their individual needs.
By prioritizing patient-centered care, managers can significantly enhance overall satisfaction and outcomes.
30. How do you approach staffing challenges in a healthcare facility?
Addressing staffing challenges involves a strategic approach:
- Assessing needs: Regularly evaluate staffing levels against patient care demands to identify shortfalls.
- Recruitment strategies: Utilize diverse recruitment channels to attract qualified candidates and promote a positive workplace culture.
- Retention efforts: Implement programs to improve job satisfaction, such as offering professional development and work-life balance initiatives.
- Flexible staffing solutions: Consider temporary or part-time staff to meet fluctuating demands.
By proactively managing staffing challenges, healthcare managers can ensure high-quality care delivery.
31. What methods do you use to evaluate the performance of healthcare staff?
Evaluating healthcare staff performance involves several effective methods:
- Regular performance reviews: Conduct scheduled evaluations based on objective criteria and job responsibilities.
- Patient feedback: Incorporate patient satisfaction scores and feedback as part of the evaluation process.
- Peer evaluations: Encourage team members to provide constructive feedback to promote a culture of collaboration.
- Continuous education: Monitor participation in professional development and training programs.
By using a comprehensive evaluation approach, managers can identify strengths and areas for improvement among staff.
32. How do you handle budget cuts in a healthcare organization?
Handling budget cuts requires careful planning and communication:
- Prioritize services: Assess which services are essential and should be maintained despite budget constraints.
- Engage stakeholders: Communicate transparently with staff and stakeholders about the reasons for cuts and their implications.
- Explore cost-saving measures: Identify non-critical expenditures that can be reduced or eliminated.
- Seek alternative funding: Look for grants, partnerships, or community support to bridge financial gaps.
Through strategic management and open communication, managers can navigate budget cuts while minimizing their impact on patient care.
33. What are the challenges of managing a diverse healthcare team?
Managing a diverse healthcare team presents unique challenges, including:
- Cultural differences: Team members may have varying communication styles and cultural practices that can lead to misunderstandings.
- Conflict resolution: Diverse perspectives can sometimes result in conflicts that need to be managed sensitively.
- Inclusivity: Ensuring all team members feel valued and included in decision-making processes can be challenging.
- Training needs: Providing tailored training that meets the diverse needs of staff can require additional resources.
By fostering an inclusive environment and promoting open dialogue, managers can turn these challenges into strengths.
34. How do you ensure quality improvement in healthcare services?
Ensuring quality improvement involves implementing systematic processes:
- Data collection: Regularly gather and analyze data related to patient outcomes and service quality.
- Setting benchmarks: Establish clear performance metrics for staff and departments.
- Continuous training: Offer ongoing education and training to keep staff updated on best practices.
- Patient involvement: Engage patients in feedback processes to help identify areas for improvement.
Through these methods, managers can foster a culture of continuous improvement and high-quality healthcare delivery.
35. Discuss the importance of emergency preparedness in healthcare management.
Emergency preparedness is critical in healthcare management because it ensures that facilities can respond effectively to crises. This includes natural disasters, pandemics, or mass casualty incidents. Key aspects include:
- Developing response plans: Create comprehensive plans that outline roles, procedures, and resource allocation during emergencies.
- Training staff: Regularly train staff on emergency protocols and conduct drills to ensure readiness.
- Resource management: Maintain an inventory of necessary supplies and equipment for emergencies.
- Community collaboration: Partner with local agencies and organizations to enhance response capabilities.
By prioritizing emergency preparedness, healthcare managers can safeguard both staff and patients during critical situations.
Below are intermediate interview questions specifically tailored for candidates applying for the position of Medicine and Health Services Manager. These questions focus on practical applications, best practices, and real-world scenarios relevant to the role.
39. What are the key roles and responsibilities of a Medicine and Health Services Manager?
A Medicine and Health Services Manager is responsible for planning, directing, and coordinating healthcare services. Key roles include managing staff, overseeing budgets, ensuring compliance with healthcare regulations, and improving patient care quality. They also work on strategic planning, implementing health programs, and collaborating with medical professionals to enhance operational efficiency and service delivery.
40. How do you ensure compliance with healthcare regulations?
Ensuring compliance with healthcare regulations involves several strategies:
- Regular training: Provide continuous education for staff about current regulations and policies.
- Audits: Conduct regular internal audits to assess compliance and identify areas for improvement.
- Documentation: Maintain accurate records of policies, procedures, and compliance activities.
- Collaboration: Work closely with legal and regulatory experts to stay updated on changes in laws.
By implementing these strategies, a manager can effectively mitigate compliance risks and enhance overall operational integrity.
41. Describe a situation where you had to handle a conflict between medical staff and administration. How did you resolve it?
In a previous role, a conflict arose over staffing levels affecting patient care. I facilitated a meeting between the medical staff and administration to discuss concerns openly. By encouraging each party to express their viewpoints, we identified common goals: improving patient care and optimizing resources. We then developed a staffing plan that balanced the needs of the staff while addressing administrative constraints, which led to a more collaborative environment.
42. What metrics do you use to evaluate the performance of a healthcare facility?
Evaluating the performance of a healthcare facility involves several key metrics:
- Patient Satisfaction Scores: Reflects the quality of care and service delivery.
- Operational Efficiency: Metrics such as average patient wait times and bed occupancy rates.
- Financial Performance: Revenue cycle metrics, including accounts receivable days and profit margins.
- Clinical Outcomes: Rates of hospital-acquired infections, readmissions, and patient safety incidents.
These metrics provide a comprehensive view of the facility’s performance, enabling informed decision-making to enhance service delivery.
43. How do you approach budgeting and financial management in a healthcare setting?
Effective budgeting in healthcare requires careful planning and monitoring. My approach includes:
- Assessing historical data: Review previous budgets to identify trends in expenses and revenues.
- Involving stakeholders: Collaborate with department heads to gather input on anticipated needs and costs.
- Setting clear objectives: Align the budget with the facility’s strategic goals and priorities.
- Regular reviews: Monitor financial performance throughout the year to make adjustments as necessary.
This proactive approach helps ensure financial stability while supporting quality patient care.
44. What strategies do you implement to improve patient care quality?
Improving patient care quality involves a multi-faceted approach:
- Education and Training: Regularly train staff on best practices and updated protocols.
- Patient Feedback: Actively seek and analyze patient feedback to identify areas for improvement.
- Quality Assurance Programs: Implement evidence-based practices and conduct regular assessments.
- Interdisciplinary Collaboration: Foster teamwork among various departments to enhance comprehensive care.
These strategies collectively contribute to enhanced patient outcomes and satisfaction.
45. How do you manage changes in healthcare policies and systems?
Managing changes in healthcare policies requires adaptability and proactive communication. I stay informed through continuous education, professional networks, and regulatory updates. Upon identifying changes, I assess their impact on operations and develop an implementation plan. Key steps include training staff, updating protocols, and monitoring compliance. Effective communication throughout the organization helps ensure a smooth transition and minimizes disruption.
46. Can you discuss a successful project you led that improved operational efficiency?
In a previous role, I led a project to streamline the patient intake process. We analyzed existing workflows and identified bottlenecks that increased wait times. By implementing a new electronic health record (EHR) system that allowed for pre-registration, we reduced the intake time by 30%. This involved training staff and restructuring the intake team. The success of this project was reflected in improved patient satisfaction scores and enhanced operational efficiency.
Medicine and Health Services Manager Interview Questions for Experienced
This set of interview questions for Medicine and Health Services Managers focuses on advanced topics relevant to experienced professionals. Questions cover areas such as strategic planning, regulatory compliance, patient care optimization, and leadership skills necessary for managing complex healthcare environments.
47. How do you ensure compliance with healthcare regulations in your organization?
Ensuring compliance with healthcare regulations involves implementing a comprehensive compliance program that includes regular training and audits. Key steps include:
- Staying updated on local, state, and federal regulations to ensure all practices align.
- Conducting regular training sessions for staff to reinforce compliance policies.
- Implementing an audit system to monitor adherence to regulations and rectify any discrepancies.
By fostering a culture of compliance and accountability, organizations can mitigate risks and improve patient safety.
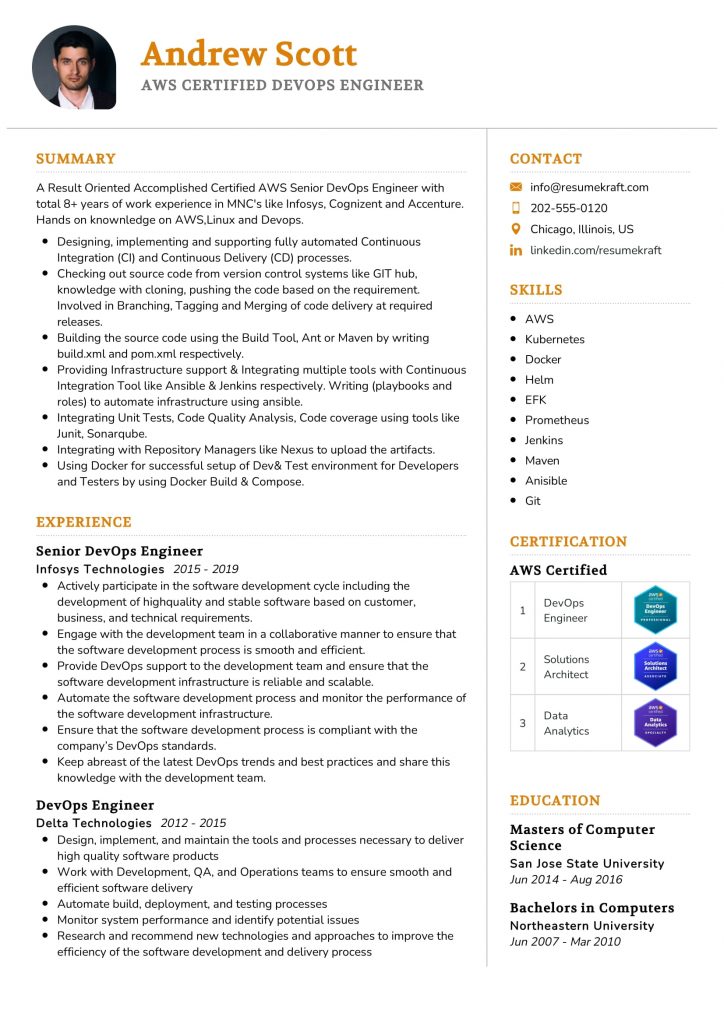
Build your resume in 5 minutes
Our resume builder is easy to use and will help you create a resume that is ATS-friendly and will stand out from the crowd.
48. What strategies do you use to optimize patient care delivery?
To optimize patient care delivery, I focus on integrating technology, streamlining processes, and enhancing team collaboration. Strategies include:
- Implementing electronic health records (EHR) to improve data accessibility and communication.
- Establishing interdisciplinary care teams to ensure holistic patient management.
- Utilizing patient feedback to continuously refine services and address concerns.
These approaches facilitate timely and effective patient care while improving overall satisfaction.
49. Can you describe your experience with budget management in a healthcare setting?
My experience with budget management includes developing, monitoring, and adjusting budgets to align with strategic goals. I utilize financial forecasting and data analysis to identify trends and areas for cost reduction. Collaboration with department heads ensures that each unit operates within its budget while still meeting patient care objectives. Regular financial reviews help maintain fiscal responsibility and accountability.
50. How do you approach leadership and mentoring within your team?
Effective leadership and mentoring involve fostering a supportive environment that encourages professional growth. I prioritize regular one-on-one check-ins to discuss career goals and provide constructive feedback. Mentorship programs are implemented to pair less experienced staff with seasoned professionals. Additionally, I promote continuous learning by offering access to training and development resources.
51. What role does data analytics play in decision-making in healthcare management?
Data analytics is crucial for informed decision-making in healthcare management. It enables organizations to:
- Identify trends in patient outcomes and operational efficiency.
- Assess the effectiveness of programs and interventions through performance metrics.
- Predict patient needs and resource allocation based on historical data.
By leveraging analytics, healthcare managers can make evidence-based decisions that enhance service delivery and patient care.
52. Describe a time when you had to implement a new technology in your organization.
In my previous role, I led the implementation of a new EHR system. This involved conducting needs assessments, selecting the appropriate technology, and developing a detailed rollout plan. I organized training sessions for staff to ensure smooth adoption and addressed any concerns proactively. Post-implementation, I gathered feedback to make necessary adjustments, resulting in improved patient data management and communication.
53. How do you manage conflicts within your healthcare team?
Managing conflicts within a healthcare team requires a proactive and empathetic approach. I encourage open communication to address issues as they arise. Conflict resolution strategies include:
- Facilitating discussions to understand different perspectives.
- Encouraging collaborative problem-solving to find mutually beneficial solutions.
- Providing mediation when necessary to ensure fairness.
By promoting a culture of respect and understanding, conflicts can be resolved constructively.
54. What is your experience with strategic planning in healthcare?
My experience with strategic planning involves conducting thorough market analyses and stakeholder assessments to inform long-term goals. I develop comprehensive action plans that outline objectives, timelines, and resource allocation. Engaging team members in the planning process fosters buy-in and ensures alignment with organizational values. Regularly reviewing and adjusting the strategy based on performance metrics is essential for achieving success.
55. How do you prioritize patient safety in your management practices?
Prioritizing patient safety is fundamental to my management practices. I implement protocols that emphasize safety, including:
- Regular training and drills for staff on safety procedures.
- Establishing a reporting system for incidents and near misses to learn from mistakes.
- Conducting safety audits to identify and mitigate potential risks.
By creating a culture of safety, we can enhance patient trust and care quality.
56. Can you discuss your experience with regulatory compliance audits?
I have led multiple regulatory compliance audits, which included preparing documentation, coordinating with auditors, and implementing corrective actions for any identified gaps. This process involves thorough preparation, including staff training, data collection, and risk assessment. Post-audit, I focus on continuous improvement by addressing findings and ensuring that our practices align with the latest regulations, thereby enhancing overall compliance.
57. What methods do you use to evaluate the effectiveness of healthcare programs?
To evaluate the effectiveness of healthcare programs, I utilize a combination of quantitative and qualitative methods, including:
- Patient satisfaction surveys to gather feedback and assess service quality.
- Key performance indicators (KPIs) to measure outcomes against predefined benchmarks.
- Cost-effectiveness analyses to determine the financial impact of programs.
These evaluations inform future program adjustments and resource allocation decisions.
58. Describe how you handle budget cuts or financial constraints in your organization.
Handling budget cuts requires strategic prioritization and clear communication. I analyze all programs to identify non-essential expenditures while preserving critical services. Engaging staff in budget discussions fosters transparency and may lead to innovative cost-saving solutions. Additionally, I explore alternative funding sources and partnerships to mitigate the impact of financial constraints on patient care.
59. How do you stay current with advancements in healthcare management?
Staying current with advancements in healthcare management involves continuous professional development. I regularly attend industry conferences, participate in webinars, and subscribe to relevant journals. Networking with peers and engaging in professional organizations also provide valuable insights and best practices. This commitment to learning ensures that I can implement innovative solutions that enhance organizational effectiveness.
60. What strategies do you employ to foster collaboration among different departments?
To foster collaboration among departments, I implement strategies that promote communication and teamwork, such as:
- Regular interdisciplinary meetings to discuss shared goals and challenges.
- Creating cross-departmental projects to encourage collaboration on common objectives.
- Establishing clear roles and responsibilities to avoid overlaps and misunderstandings.
These strategies strengthen relationships and improve overall organizational performance.
Here are some interview questions tailored for experienced candidates applying for the role of Medicine and Health Services Manager. These questions focus on critical aspects such as architecture, optimization, scalability, design patterns, and leadership.
62. How do you approach optimizing healthcare operations in a facility?
Optimizing healthcare operations involves several strategic approaches:
- Data Analysis: Utilize data analytics to identify bottlenecks and inefficiencies in patient flow and resource allocation.
- Process Improvement: Implement Lean and Six Sigma methodologies to streamline processes and reduce waste.
- Technology Integration: Leverage electronic health records (EHR) and other technologies to enhance communication and coordination among staff.
- Staff Training: Invest in training programs to ensure staff are knowledgeable about best practices and efficient workflows.
These strategies collectively enhance operational efficiency, leading to improved patient care and satisfaction.
63. Can you explain the significance of scalable health information systems?
Scalable health information systems are crucial for several reasons:
- Adaptability: They can accommodate increasing amounts of data as the organization grows, ensuring that patient information is always accessible.
- Cost Efficiency: Scalable systems reduce the need for frequent upgrades or complete overhauls, saving costs in the long run.
- Improved Patient Care: As systems scale, they allow for better data analysis, leading to more informed decision-making and improved patient outcomes.
- Interoperability: Scalable systems facilitate integration with other healthcare providers and systems, enhancing collaborative care.
This adaptability is essential in addressing both current demands and future healthcare challenges.
64. What design patterns do you find most effective in managing healthcare projects?
In managing healthcare projects, several design patterns are particularly effective:
- Microservices: This pattern allows for breaking down applications into smaller, independent services, making it easier to manage and scale.
- Service-Oriented Architecture (SOA): SOA promotes reusability and interoperability among different health systems, ensuring seamless data exchange.
- Event-Driven Architecture: This pattern facilitates real-time data processing and responsiveness, which is critical in emergency healthcare situations.
- Repository Pattern: Useful for abstracting data access, it simplifies data management and enhances performance across different modules.
Utilizing these design patterns can significantly improve project outcomes by enhancing flexibility and responsiveness to changes in healthcare needs.
65. How do you mentor your team to enhance their leadership skills in a healthcare setting?
Mentoring a team to enhance leadership skills involves several key strategies:
- Individual Development Plans: Work with team members to create personalized plans that focus on their specific leadership goals and areas for improvement.
- Encourage Cross-Training: Allow team members to take on different roles and responsibilities, fostering a broader understanding of the healthcare environment.
- Provide Constructive Feedback: Regular feedback sessions help team members understand their strengths and areas for growth.
- Lead by Example: Demonstrate effective leadership behaviors in your own actions to inspire and guide your team.
These mentoring approaches create a supportive environment that encourages team members to develop their leadership capabilities, ultimately benefiting the organization.
How to Prepare for Your Medicine and Health Services Manager Interview
Preparing for a Medicine and Health Services Manager interview requires a strategic approach. Focus on understanding healthcare regulations, financial management, and leadership skills to effectively demonstrate your capability to oversee medical facilities and improve patient care quality during the interview.
- Research Healthcare Trends: Stay updated on current trends in healthcare, such as telemedicine and value-based care. Understanding these topics shows your commitment to the field and prepares you to discuss their implications on management strategies during the interview.
- Familiarize with Regulations: Review key healthcare regulations and policies, including HIPAA and the Affordable Care Act. Being knowledgeable about these laws will help you articulate your understanding of compliance and patient advocacy, which are crucial in the role.
- Prepare Leadership Examples: Reflect on your past experiences that highlight your leadership skills, particularly in managing teams or projects. Prepare specific examples that demonstrate your ability to motivate staff and improve operational efficiency in healthcare settings.
- Understand Financial Management: Brush up on budgeting, financial analysis, and resource allocation. Be ready to discuss how you’ve managed budgets or improved financial performance in previous roles, as financial acumen is essential for this position.
- Develop Problem-Solving Scenarios: Think of potential challenges a Medicine and Health Services Manager might face, such as staffing shortages or regulatory changes. Prepare to discuss how you would approach solving these issues, showcasing your critical thinking and strategic planning abilities.
- Practice Behavioral Interview Questions: Expect behavioral questions that assess your past experiences and decision-making skills. Use the STAR method (Situation, Task, Action, Result) to structure your responses, ensuring clarity and relevance to the role.
- Network with Professionals: Connect with current or former Medicine and Health Services Managers to gain insights into their experiences and advice. Networking can provide you with valuable information on what to expect in the interview and emerging trends in the field.
Common Medicine and Health Services Manager Interview Mistakes to Avoid
Interviewing for a Medicine and Health Services Manager position requires careful preparation. Avoiding common mistakes can significantly improve your chances of success. Here are eight pitfalls to watch out for during your interview process.
- Inadequate Knowledge of Healthcare Regulations: Failing to demonstrate understanding of healthcare laws and regulations can signal a lack of preparedness. Familiarity with HIPAA, Medicare, and state-specific policies is crucial for this role.
- Neglecting Soft Skills: While technical skills are important, this role demands strong communication, leadership, and conflict-resolution skills. Neglecting to highlight these can lead interviewers to doubt your suitability for team management.
- Not Researching the Organization: Entering an interview without knowledge of the organization’s mission, values, and recent developments can convey a lack of interest. Researching beforehand shows commitment and helps tailor your responses.
- Ignoring Behavioral Questions: Many interviews include behavioral questions to assess how you’ve handled past situations. Failing to prepare examples using the STAR method (Situation, Task, Action, Result) can weaken your responses.
- Overemphasizing Technical Skills: While technical expertise is important, focusing solely on it overlooks the managerial aspect of the role. Balance your technical knowledge with discussions about team management and strategic planning.
- Being Unprepared for Questions about Leadership: Expect questions about your leadership style and experiences. Not having specific examples ready can make you seem unqualified for a management position.
- Failure to Ask Questions: Not asking questions can indicate a lack of interest or engagement. Prepare thoughtful questions about the organization’s challenges or goals to demonstrate your enthusiasm and critical thinking.
- Not Following Up: Neglecting to send a thank-you email or follow-up message can leave a negative impression. A well-crafted follow-up reinforces your interest and professionalism, keeping you in the interviewer’s mind.
Key Takeaways for Medicine and Health Services Manager Interview Success
- Prepare a strong resume using an AI resume builder to highlight your skills and experiences relevant to Medicine and Health Services Management, ensuring clarity and professionalism in presentation.
- Utilize well-structured resume templates to organize your information effectively, making it easy for interviewers to assess your qualifications at a glance.
- Showcase your experiences through specific resume examples that demonstrate your achievements and contributions in previous roles, emphasizing results in healthcare settings.
- Craft personalized cover letters that align your career goals with the organization’s mission, highlighting your passion for enhancing health services management.
- Engage in mock interview practice to build confidence and refine your responses, ensuring you are well-prepared to articulate your vision and strategies during the actual interview.
Frequently Asked Questions
1. How long does a typical Medicine and Health Services Manager interview last?
A typical interview for a Medicine and Health Services Manager position usually lasts between 30 to 60 minutes. The duration can vary depending on the organization and the interview format. Expect questions that assess both your technical knowledge and soft skills, including leadership and problem-solving abilities. It’s important to prepare for both behavioral and situational questions during this time, as interviewers often seek to understand how you would handle various challenges in a healthcare setting.
2. What should I wear to a Medicine and Health Services Manager interview?
For a Medicine and Health Services Manager interview, it is advisable to dress in professional business attire. This typically means a suit or blazer paired with dress pants or a skirt. Women may opt for a professional dress or blouse with dress pants. Aim for neutral colors and avoid overly flashy accessories. Your appearance should reflect your professionalism and respect for the healthcare industry, which values a polished and competent image.
3. How many rounds of interviews are typical for a Medicine and Health Services Manager position?
<pTypically, candidates for a Medicine and Health Services Manager position can expect two to three rounds of interviews. The first round is often a phone or video interview focused on initial qualifications and fit. Subsequent rounds may involve in-person interviews with hiring managers, team members, and possibly executive leadership. Each round often dives deeper into your experience, leadership style, and problem-solving capabilities, so be prepared to discuss your resume and relevant scenarios in detail.4. Should I send a thank-you note after my Medicine and Health Services Manager interview?
Yes, sending a thank-you note after your interview is highly recommended. It shows appreciation for the interviewer’s time and reinforces your interest in the position. Aim to send your note within 24 hours of the interview, highlighting specific points discussed that you found particularly engaging. A thoughtful thank-you can leave a positive impression and differentiate you from other candidates, underscoring your professionalism and enthusiasm for the role in healthcare management.