Preparing for a Band 6 Nurse interview is a crucial step in advancing your nursing career. This role is unique as it bridges the gap between junior nurses and senior leadership, requiring a blend of clinical expertise, leadership skills, and effective communication. Proper interview preparation is essential, as it not only boosts your confidence but also helps you articulate your experiences and demonstrate your suitability for the role. In this comprehensive guide, we will cover common interview questions, effective strategies for answering them, tips for showcasing your skills and experiences, and ways to present yourself as the ideal candidate for a Band 6 Nurse position.
What to Expect in a Band 6 Nurse Interview
In a Band 6 Nurse interview, candidates can expect a structured format that typically includes a panel of interviewers, often comprising senior nursing staff, nurse managers, and human resources personnel. The interview may consist of competency-based questions, situational judgment scenarios, and discussions about clinical experience. Candidates should be prepared to demonstrate their clinical knowledge, leadership qualities, and ability to work within a multidisciplinary team. The process may also include practical assessments or role-playing exercises to evaluate clinical skills and decision-making abilities in real-life scenarios.
Band 6 Nurse Interview Questions For Freshers
These Band 6 Nurse interview questions are tailored for freshers entering the nursing field. Candidates should master fundamental concepts such as patient care, clinical procedures, and effective communication to demonstrate their readiness for the role.
1. What are the key responsibilities of a Band 6 Nurse?
A Band 6 Nurse typically has responsibilities that include managing a team of junior nurses, overseeing patient care, ensuring compliance with healthcare standards, and contributing to the development of nursing practices. They also play a critical role in patient assessment, care planning, and collaboration with multidisciplinary teams to enhance patient outcomes.
2. How do you prioritize patient care in a busy ward?
Prioritizing patient care involves assessing the severity of patients’ conditions and the urgency of their needs. A Band 6 Nurse should use tools like the ABCDE approach (Airway, Breathing, Circulation, Disability, Exposure) to identify critical issues and prioritize interventions. Delegating tasks effectively and communicating with the team are also essential for managing a busy environment.
3. What is your approach to handling difficult patients?
Handling difficult patients requires empathy and effective communication. It is important to remain calm, listen actively to their concerns, and validate their feelings. Establishing rapport can help de-escalate tense situations. If necessary, involving a senior nurse or other healthcare professionals can provide additional support for managing challenging behaviors.
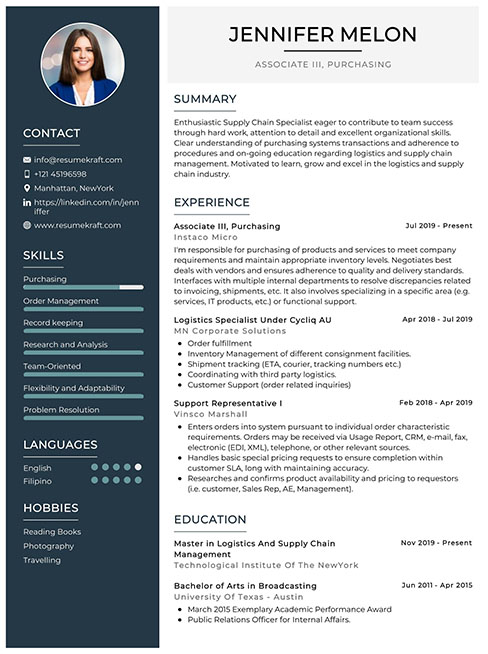
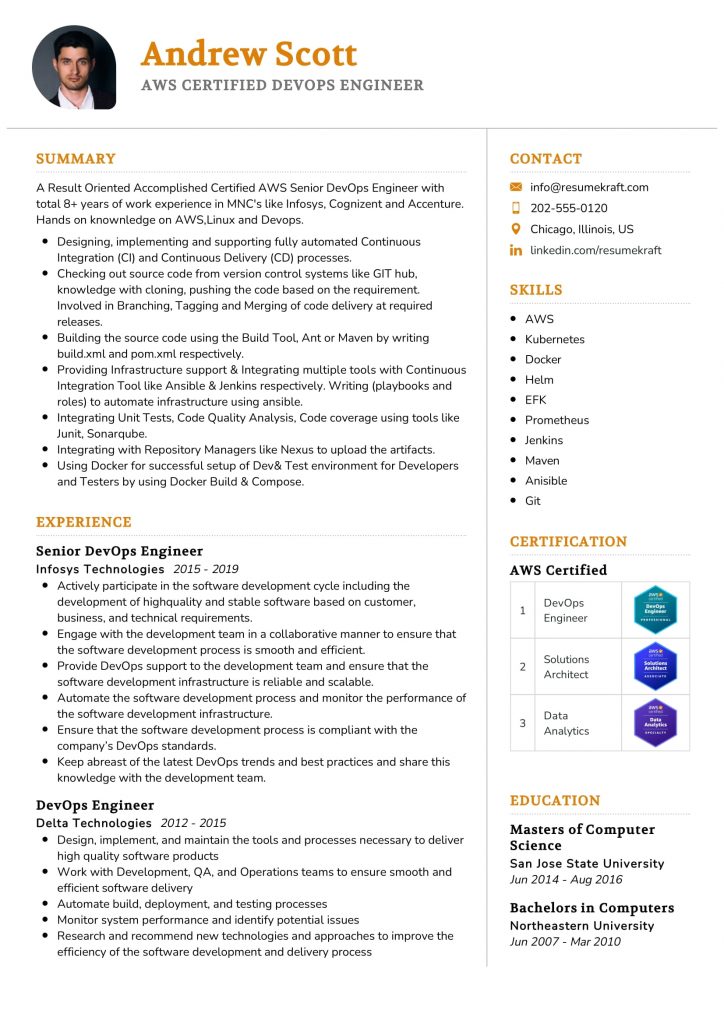
Build your resume in just 5 minutes with AI.
4. Describe your experience with electronic health records (EHR).
While I may not have extensive experience, I have completed training in using electronic health records. I understand how to document patient information accurately, access medical history, and input care plans. Familiarity with EHR systems enhances efficiency and reduces errors in patient care documentation, which is crucial in modern healthcare settings.
5. How do you ensure effective communication with your team?
- Regular Meetings: Holding brief daily huddles to discuss patient care and updates fosters open lines of communication.
- Feedback: Encouraging team members to share feedback helps improve communication styles and ensures everyone is heard.
- Documentation: Clearly documenting patient care plans and updates in shared systems helps keep everyone informed.
Effective communication is vital for teamwork and delivering high-quality patient care.
6. What strategies do you use for patient education?
Patient education is crucial for promoting health literacy. Strategies include using simple language, demonstrating procedures, providing written materials, and encouraging questions to ensure understanding. Tailoring education to the patient’s level of comprehension and cultural background enhances the effectiveness of the information shared.
7. How do you manage stress in a high-pressure environment?
Managing stress involves maintaining a healthy work-life balance, practicing mindfulness techniques, and seeking support from colleagues. Regularly taking short breaks during shifts can help recharge. Additionally, engaging in professional development and pursuing stress management training can provide tools to cope with the demands of nursing.
8. Can you describe a situation where you had to advocate for a patient?
Advocating for a patient may involve identifying their needs when they are unable to communicate effectively. For example, if a patient expresses discomfort but is unable to articulate their pain level, I would assess their non-verbal cues, communicate with the medical team about their needs, and ensure appropriate pain management is initiated promptly.
9. What is the importance of infection control in nursing?
- Patient Safety: Infection control practices prevent the spread of infections within healthcare settings, protecting vulnerable patients.
- Compliance: Adhering to infection control protocols is a legal and ethical responsibility for healthcare professionals.
- Quality of Care: Effective infection control contributes to better patient outcomes and reduces healthcare-associated infections.
Ultimately, infection control is fundamental in maintaining a safe healthcare environment.
10. Describe your experience with wound care.
In my training, I have learned about various wound types and their management. This includes cleaning, dressing techniques, and recognizing signs of infection. I understand the importance of assessing the wound regularly and collaborating with other healthcare professionals to develop an effective care plan. Continuing education is essential to stay updated on best practices.
11. How do you handle medication administration safely?
- Five Rights: Always adhere to the five rights of medication administration: right patient, right drug, right dose, right route, and right time.
- Double-Check: Always double-check medications with a colleague when in doubt, especially with high-risk medications.
- Documentation: Accurately document all medication given to ensure patient safety and compliance.
Following these practices minimizes the risk of medication errors and enhances patient safety.
12. What role does teamwork play in nursing?
Teamwork is crucial in nursing as it ensures comprehensive patient care. Collaborative efforts among nurses, doctors, and allied health professionals contribute to better decision-making and improved patient outcomes. Effective teamwork allows for sharing of knowledge, skills, and resources, which can enhance productivity and job satisfaction while minimizing errors.
13. How do you keep yourself updated with nursing practices?
- Continuing Education: Enrolling in courses and attending workshops helps expand my knowledge and skills.
- Professional Journals: Reading nursing journals and articles keeps me informed about the latest research and best practices.
- Networking: Engaging with other healthcare professionals and participating in forums helps share insights and experiences.
Staying updated is essential to provide the best care to patients and remain competent in the field.
14. How would you approach a situation where a colleague is not following protocols?
If I observe a colleague not following protocols, I would address the situation directly and respectfully. I would approach them privately to discuss my observations, ensuring to listen to their perspective. If the behavior continues or poses a risk to patient safety, I would escalate the matter to a supervisor for further action, prioritizing patient safety above all.
15. What is your understanding of patient confidentiality?
Patient confidentiality refers to the ethical and legal obligation to protect patients’ personal health information. This includes not disclosing any information without consent, ensuring secure handling of records, and discussing patient cases only in appropriate settings. Upholding confidentiality is fundamental in building trust and maintaining professionalism in nursing practice.
These questions are tailored for Band 6 Nurse freshers and focus on essential nursing concepts and practices they should be familiar with as they begin their careers.
16. What are the key responsibilities of a Band 6 nurse?
A Band 6 nurse typically has a range of responsibilities including supervising junior staff, managing a team, and ensuring high standards of patient care. They are also involved in assessing patient needs, planning and implementing care plans, and evaluating patient outcomes. Additionally, they may take on leadership roles in clinical practice, contribute to service development, and participate in training and mentoring staff.
17. How do you prioritize patient care in a busy environment?
Prioritizing patient care in a busy environment requires effective time management and critical thinking skills. Nurses should assess the urgency of each patient’s needs based on their condition, the severity of symptoms, and potential complications. Key strategies include:
- Using a triage system to categorize patients based on their immediate needs.
- Communicating with the healthcare team to delegate tasks effectively.
- Regularly reviewing and adjusting priorities as situations change.
This approach ensures that the most critical patients receive timely and appropriate care.
18. What is the importance of patient confidentiality and how do you ensure it?
Patient confidentiality is vital in nursing as it builds trust between patients and healthcare providers. It protects patient privacy and adheres to legal and ethical standards. To ensure confidentiality, nurses should:
- Only share patient information with authorized personnel.
- Securely store patient records and use password protection for electronic data.
- Educate patients about their rights regarding their information.
Maintaining confidentiality fosters a safe environment for patients to discuss their concerns openly.
19. Can you explain the nursing process and its steps?
The nursing process is a systematic approach to providing patient care and consists of five key steps:
- Assessment: Collecting comprehensive data about the patient’s health status.
- Diagnosis: Analyzing assessment data to identify patient problems.
- Planning: Developing a care plan with measurable goals and interventions.
- Implementation: Executing the care plan and providing interventions.
- Evaluation: Assessing the patient’s response to the interventions and modifying the plan as needed.
This structured process helps ensure effective and holistic nursing care.
20. What is the significance of evidence-based practice in nursing?
Evidence-based practice (EBP) is crucial in nursing as it integrates clinical expertise, patient values, and the best research evidence to guide decision-making. The significance of EBP includes:
- Improving patient outcomes through the use of proven interventions.
- Enhancing the quality of care by incorporating the latest research findings.
- Fostering a culture of continuous improvement and professional development among nursing staff.
By applying EBP, nurses can provide safe, effective, and high-quality care tailored to individual patient needs.
21. How do you handle difficult conversations with patients or families?
Handling difficult conversations with patients or families requires empathy, active listening, and clear communication. Key steps include:
- Creating a supportive environment where patients feel safe to express their feelings.
- Using clear and simple language to explain complex medical information.
- Listening actively to their concerns without interrupting, and acknowledging their emotions.
- Providing honest and compassionate responses while offering support and resources.
This approach helps to build trust and ensures that patients and families feel heard and respected during challenging discussions.
Band 6 Nurse Intermediate Interview Questions
Band 6 Nurse interview questions focus on both clinical skills and leadership abilities. Candidates should be prepared to discuss patient care management, team collaboration, and the implementation of evidence-based practices. Understanding mid-level concepts such as risk assessment, communication strategies, and quality improvement is essential for success in these interviews.
22. What strategies do you use for effective communication with patients and their families?
Effective communication is crucial in nursing for building trust and ensuring understanding. I employ strategies such as active listening, using clear and simple language, and encouraging questions. Additionally, I adapt my communication style to the patient’s needs, whether that involves using visual aids for those with hearing impairments or ensuring that non-English speakers have access to interpreters. This personalized approach helps in fostering a supportive environment.
23. How do you prioritize tasks in a busy environment?
Prioritizing tasks in a busy nursing environment involves assessing patient needs, urgency of care, and available resources. I use a systematic approach such as the ABC prioritization method (Airway, Breathing, Circulation) and the nursing process (Assessment, Diagnosis, Planning, Implementation, Evaluation). This helps ensure that critical tasks are addressed first while maintaining overall care quality.
24. Can you describe a time when you had to handle a difficult patient situation?
In a previous role, I encountered a patient who was non-compliant with their medication regimen due to side effects. I took the time to listen to their concerns and collaborated with the physician to adjust their medications. By involving the patient in the decision-making process, we reached a satisfactory resolution, improving their adherence and overall health outcomes.
25. What is your approach to patient education?
My approach to patient education involves assessing the patient’s knowledge level and learning preferences. I provide information in a clear, concise manner, utilizing teach-back methods to ensure comprehension. Additionally, I offer written materials and resources for further learning, encourage questions, and follow up with patients to reinforce their understanding and address any ongoing concerns.
26. How do you ensure compliance with infection control measures?
Compliance with infection control measures is ensured through regular training, adherence to protocols, and monitoring practices. I emphasize hand hygiene, the use of personal protective equipment (PPE), and proper sterilization techniques. I also conduct audits and feedback sessions with the team to reinforce the importance of infection control, which helps maintain a safe environment for patients and staff.
27. Describe your experience with electronic health records (EHR).
I have extensive experience with EHR systems, which I use for documenting patient assessments, care plans, and medication administration. I ensure accurate and timely entries to promote continuity of care and facilitate communication among the healthcare team. Additionally, I am proficient in utilizing EHR tools for tracking patient outcomes and quality metrics, enhancing overall patient safety.
28. What role do you believe nurses play in patient advocacy?
Nurses play a vital role in patient advocacy by ensuring that patients’ rights and preferences are respected. This involves actively listening to patients, providing them with information about their care options, and representing their interests within the healthcare team. By advocating for patients, nurses help ensure equitable access to care and contribute to better health outcomes.
29. How do you handle conflicts within a healthcare team?
Handling conflicts within a healthcare team requires open communication and collaboration. I approach conflicts by first addressing the issue directly with the involved parties to understand differing perspectives. I encourage a solution-oriented dialogue, aiming for a compromise that upholds patient care standards. If necessary, I involve a supervisor or mediator to facilitate resolution and maintain team cohesion.
30. What measures do you take to provide culturally competent care?
Providing culturally competent care involves understanding and respecting patients’ cultural backgrounds and beliefs. I take measures such as participating in cultural competency training, actively seeking to learn about different cultures, and using interpreters when needed. By incorporating culturally relevant practices into patient care, I can improve patient satisfaction and health outcomes.
31. How do you approach quality improvement initiatives?
I approach quality improvement initiatives through data analysis, stakeholder engagement, and evidence-based practices. By identifying areas for improvement, I collaborate with the team to develop measurable goals and implement changes. I also monitor outcomes and gather feedback to evaluate the effectiveness of interventions, ensuring continuous improvement in patient care and safety.
32. Can you explain the importance of mental health assessments in nursing?
Mental health assessments are crucial in nursing as they help identify patients’ psychological needs and risks. By incorporating mental health evaluations into patient care, I can recognize conditions such as anxiety or depression that may affect physical health and treatment adherence. Early identification allows for timely interventions, enhancing overall patient outcomes and quality of life.
33. What is your experience with medication management?
My experience with medication management includes administering medications, monitoring for side effects, and educating patients about their prescriptions. I ensure accuracy by cross-checking dosages and patient records, and I advocate for patients by involving them in discussions about their medication regimens. This holistic approach helps promote adherence and safe medication practices.
34. How do you deal with stress in a high-pressure environment?
Dealing with stress in a high-pressure environment involves effective time management, self-care practices, and seeking support from colleagues. I prioritize tasks to maintain focus and utilize relaxation techniques such as deep breathing during busy shifts. Additionally, I make it a point to debrief with team members after challenging situations to process experiences and foster a supportive atmosphere.
35. Describe your experience with interprofessional collaboration.
I have significant experience with interprofessional collaboration, working closely with physicians, pharmacists, and other healthcare providers to deliver comprehensive care. Effective communication and mutual respect are key components of successful collaboration. I participate in multidisciplinary rounds and case discussions to ensure that all aspects of patient care are considered, ultimately leading to improved outcomes and patient satisfaction.
The following questions are tailored for intermediate-level Band 6 Nurse candidates, focusing on practical applications, best practices, and real-world scenarios they may encounter in their nursing careers.
37. How do you prioritize patient care in a busy ward?
Prioritizing patient care in a busy ward involves assessing the urgency and severity of patients’ conditions. The ABCDE approach (Airway, Breathing, Circulation, Disability, Exposure) helps in determining the priorities. Additionally, communication with the healthcare team is crucial to delegate tasks effectively. Regularly reviewing patient status and being adaptable to changes can also enhance care delivery. Utilizing tools like patient acuity scales can further assist in managing care priorities efficiently.
38. What strategies do you use to manage stress and prevent burnout in nursing?
- Self-Care: Engaging in activities outside of work, such as exercise, hobbies, and socializing, helps maintain mental health.
- Time Management: Prioritizing tasks and taking scheduled breaks can prevent overwhelming feelings and promote a balanced workload.
- Support Systems: Leaning on colleagues and participating in support groups fosters a sense of community and shared experiences.
- Mindfulness Practices: Techniques like meditation or deep-breathing exercises can reduce anxiety and improve focus during shifts.
These strategies are essential for sustaining a long and fulfilling nursing career, allowing for better patient care and personal well-being.
39. Describe a time when you had to advocate for a patient.
In a previous role, I encountered a patient who was reluctant to undergo necessary treatment due to fear of side effects. I took the initiative to have a detailed discussion with the patient, addressing their concerns and providing clear, factual information about the benefits and risks of the treatment. I also collaborated with the healthcare team to ensure the patient received additional support, such as counseling. Ultimately, the patient felt more empowered and chose to proceed with the treatment, which significantly improved their health outcomes.
40. What are the key components of effective communication with patients and their families?
- Active Listening: Ensuring that you fully understand the patient’s and family’s concerns by giving them your undivided attention.
- Clarity and Simplicity: Using clear, jargon-free language to explain medical conditions and treatment options.
- Empathy: Showing understanding and compassion towards the emotions and situations faced by patients and their families.
- Follow-Up: Providing opportunities for questions and ensuring all parties feel informed about the patient’s care plan.
Effective communication fosters trust and collaboration between healthcare providers, patients, and families, ultimately leading to improved care and satisfaction.
41. How do you handle conflicts with colleagues in a healthcare setting?
Handling conflicts with colleagues requires a calm and professional approach. I believe in addressing issues directly and respectfully. I first try to understand the other person’s perspective, which can help identify the root cause of the conflict. Open communication is key; I prefer to discuss the matter privately to avoid escalation. If needed, involving a mediator or supervisor can help facilitate a resolution. Ultimately, focusing on shared goals, such as patient care and teamwork, can help overcome interpersonal conflicts.
42. Can you explain the importance of evidence-based practice in nursing?
Evidence-based practice (EBP) is crucial in nursing as it integrates the best available research with clinical expertise and patient values. This approach ensures that patient care decisions are grounded in the most current and relevant data, leading to improved health outcomes. EBP encourages continuous learning and adaptation of best practices, promoting higher standards of care. Moreover, it empowers nurses to critically evaluate and implement new findings, enhancing the overall quality of healthcare delivery.
Band 6 Nurse Interview Questions for Experienced
This section focuses on Band 6 Nurse interview questions tailored for experienced professionals. The questions delve into advanced topics such as clinical decision-making, patient safety, leadership skills, mentoring techniques, and strategies for optimizing care delivery in a healthcare setting.
43. Can you describe a time when you had to make a critical decision in a clinical setting?
In my previous role, I encountered a patient with rapidly deteriorating vital signs. I quickly assessed the situation, gathered relevant patient history, and consulted with the attending physician. After discussing the potential interventions, we decided on immediate intubation to secure the airway. This decision was crucial in stabilizing the patient, who later required intensive care. Effective teamwork and communication were key in this scenario.
44. How do you ensure patient safety in your daily practice?
- Regularly conduct risk assessments: I consistently evaluate potential risks in my unit and implement preventative measures.
- Encourage open communication: Creating an environment where staff feel comfortable reporting concerns is essential for patient safety.
- Stay updated on protocols: I ensure that I am well-informed about the latest guidelines and best practices in nursing care.
By prioritizing these strategies, I contribute to a culture of safety that benefits both patients and staff.
45. What strategies do you use for mentoring junior nurses?
- One-on-one coaching: I conduct regular check-ins to discuss challenges and provide guidance tailored to their specific needs.
- Encourage critical thinking: I ask open-ended questions during clinical discussions to foster their problem-solving skills.
- Model best practices: Demonstrating effective techniques in real-time helps them learn through observation.
Mentoring in nursing is vital for professional growth, and I take pride in fostering confidence and competence in my colleagues.
46. How do you approach optimizing care delivery in your unit?
I start by analyzing patient flow and identifying bottlenecks in our processes. Collaborating with my team, we implement evidence-based practices to streamline procedures. For instance, we introduced standardized protocols for patient handoff, which significantly reduced miscommunication errors. Regular feedback sessions allow us to refine our approach continually, ensuring high-quality care and improved patient outcomes.
47. Can you discuss a design pattern you have implemented in your nursing practice?
A design pattern I often utilize is the “SBAR” (Situation, Background, Assessment, Recommendation) communication framework. It provides a structured method for reporting patient information, ensuring clarity and efficiency during handoffs. This pattern has led to more effective interprofessional communication and a reduction in errors during transitions of care, ultimately enhancing patient safety.
Build your resume in 5 minutes
Our resume builder is easy to use and will help you create a resume that is ATS-friendly and will stand out from the crowd.
48. Describe how you handle conflicts within your team.
When conflicts arise, I prioritize open dialogue between the involved parties. I facilitate a meeting to allow each person to express their concerns and viewpoints. By focusing on the issue rather than personal differences, we can collaboratively seek solutions. I believe that addressing conflicts promptly can lead to stronger teamwork and improved morale in the unit.
49. How do you stay current with advancements in nursing practice?
I actively engage in continuous professional development by attending workshops, webinars, and conferences. I also subscribe to nursing journals and participate in online forums to exchange knowledge with peers. Staying informed about the latest research and best practices allows me to integrate new techniques into my care delivery, ultimately benefiting my patients.
50. What role does leadership play in your daily nursing practice?
Leadership is integral to my practice as it sets the tone for my team’s culture and performance. I strive to be a positive role model by demonstrating accountability, effective communication, and compassion. By empowering my team members to take initiative in their roles, I foster a collaborative environment that enhances patient care and staff satisfaction.
51. How do you handle high-stress situations in the clinical environment?
- Prioritize tasks: I quickly assess the situation to determine the most urgent needs and allocate resources accordingly.
- Maintain composure: Staying calm enables me to think clearly and make informed decisions, which helps reassure the team.
- Seek support: I recognize when to involve additional team members to ensure patient safety and effective care.
By employing these strategies, I can navigate high-stress situations effectively, ensuring the best outcomes for patients and staff.
52. Can you provide an example of how you implemented a quality improvement initiative?
In my previous position, I noticed an increase in patient falls on our unit. I led a quality improvement initiative that included staff training on fall prevention strategies and the implementation of a new patient assessment tool. We tracked fall incidents before and after the initiative, resulting in a 30% decrease in falls over six months, showcasing the importance of proactive measures.
53. How do you approach patient education in your practice?
Patient education is essential for promoting health and preventing complications. I assess each patient’s understanding and tailor my teaching methods to their learning styles. I utilize teach-back techniques to ensure comprehension and provide written materials for reference. This personalized approach empowers patients to take an active role in their care, improving adherence to treatment plans.
54. What methods do you use to evaluate the effectiveness of care interventions?
- Patient feedback: I regularly solicit feedback from patients regarding their care experience, which helps identify areas for improvement.
- Outcome measurement: I track key performance indicators, such as readmission rates and patient satisfaction scores, to assess the effectiveness of interventions.
- Peer reviews: Engaging in peer evaluations fosters a culture of continuous improvement and shared learning.
By employing these methods, I can adjust my practice to ensure the highest level of care for my patients.
55. How do you ensure adherence to evidence-based practices in your unit?
I promote a culture of evidence-based practice by encouraging my team to stay informed about the latest research. We regularly hold discussions on recent studies and their implications for our care. Additionally, I collaborate with clinical leaders to develop protocols based on best practices, ensuring that our care aligns with current guidelines and improves patient outcomes.
This question is designed for experienced Band 6 Nurses and focuses on their leadership and mentoring abilities, which are critical in nursing roles.
58. How do you approach mentoring junior nursing staff in a busy clinical environment?
Mentoring junior nursing staff in a busy clinical environment requires a structured yet flexible approach. Key strategies include:
- Establishing Trust: Create a supportive atmosphere where juniors feel comfortable asking questions and expressing concerns.
- Regular Check-Ins: Schedule consistent one-on-one meetings to discuss their progress, address any challenges, and provide feedback.
- Role Modeling: Demonstrate best practices in patient care, communication, and teamwork, encouraging juniors to emulate these behaviors.
- Encouraging Independence: Gradually allow them to take on more responsibilities, fostering confidence and decision-making skills.
- Providing Resources: Share relevant literature, guidelines, and training opportunities that can enhance their knowledge and skills.
Ultimately, effective mentoring not only supports the development of junior staff but also contributes to improved patient care and team dynamics.
How to Prepare for Your Band 6 Nurse Interview
Preparing for a Band 6 Nurse interview requires a strategic approach that highlights both clinical skills and leadership capabilities. Focus on understanding the role’s expectations, demonstrating your experience, and showcasing your ability to work effectively within a multidisciplinary team.
- Familiarize Yourself with the Job Description: Review the Band 6 Nurse role specifics, including responsibilities and required competencies. Understand the clinical skills and leadership qualities expected, which will help you tailor your responses during the interview.
- Research the Healthcare Organization: Gain insight into the values, mission, and current initiatives of the organization you’re interviewing with. Understanding their culture and priorities will allow you to align your answers with their goals and demonstrate your commitment to their vision.
- Prepare for Behavioral Questions: Anticipate questions that assess your past behavior in challenging situations. Use the STAR method (Situation, Task, Action, Result) to structure your responses, ensuring you highlight your problem-solving abilities and teamwork experience.
- Review Clinical Guidelines and Protocols: Brush up on relevant clinical guidelines and protocols that pertain to the Band 6 role. Being knowledgeable about current best practices will help you answer clinical scenario questions effectively and demonstrate your expertise.
- Practice Leadership Scenarios: As a Band 6 Nurse, you’ll likely be expected to take on leadership duties. Prepare examples of situations where you’ve successfully led a team, managed conflicts, or improved patient care, showcasing your leadership skills and decision-making abilities.
- Engage in Mock Interviews: Consider conducting mock interviews with a peer or mentor to practice your responses and receive constructive feedback. This will help boost your confidence and refine your communication skills, making you more comfortable during the actual interview.
- Prepare Questions for the Interviewer: Have thoughtful questions ready to ask at the end of the interview. Inquiring about team dynamics, professional development opportunities, or challenges the unit faces demonstrates your interest in the role and helps you assess if the position is a good fit.
Common Band 6 Nurse Interview Mistakes to Avoid
Preparing for a Band 6 Nurse interview requires understanding both clinical skills and effective communication. Avoiding common mistakes can significantly enhance your chances of success and help you present your qualifications and experiences more effectively.
- Not Researching the Trust
Failing to understand the specific Trust’s values and goals can show a lack of genuine interest in the role. Researching their mission, recent projects, and challenges will demonstrate your commitment and alignment with their objectives.
- Ignoring the Job Description
Overlooking the key responsibilities and requirements outlined in the job description may lead to unpreparedness. Familiarizing yourself with these details helps you tailor your answers to highlight relevant skills and experiences.
- Underestimating the Importance of Communication Skills
As a Band 6 Nurse, strong communication is vital. Failing to effectively articulate your thoughts can hinder your ability to convey your competency in patient care and teamwork during the interview.
- Not Preparing for Behavioral Questions
Interviewers often use behavioral questions to assess your problem-solving and interpersonal skills. Not preparing examples of past experiences can leave you unable to demonstrate how you’ve handled challenges in your nursing practice.
- Being Vague About Clinical Experience
Providing vague answers about your clinical experiences can create doubts about your qualifications. Be specific about your roles, responsibilities, and the outcomes of your actions to illustrate your expertise and confidence.
- Neglecting Questions for the Interviewer
Not asking insightful questions can make you appear disinterested. Prepare thoughtful questions about the team dynamics, patient care approaches, or professional development opportunities to show your engagement and initiative.
- Failing to Highlight Leadership Skills
As a Band 6 Nurse, you are expected to exhibit leadership qualities. Neglecting to discuss your leadership experiences or how you’ve mentored others may lead to the impression that you aren’t ready for this role.
- Not Practicing Your Responses
Going into an interview without practice can result in nervousness and unclear answers. Rehearsing your responses to common nursing interview questions helps build confidence and ensures clarity in your communication.
Key Takeaways for Band 6 Nurse Interview Success
- Prepare your resume thoroughly using an AI resume builder to ensure it highlights your skills and experience effectively. Choose appropriate resume templates that align with the nursing profession.
- Showcase relevant experiences in your application by referring to strong resume examples. Tailor your achievements to demonstrate your capability for a Band 6 Nurse role.
- Craft personalized cover letters that reflect your passion for nursing and the specific position. Address how your skills align with the job requirements and the organization’s values.
- Engage in mock interview practice to build confidence and improve your responses. This will help you articulate your experiences and qualifications clearly during the actual interview.
- Research common interview questions for Band 6 Nurses, focusing on clinical scenarios and leadership skills. Prepare thoughtful answers that demonstrate your critical thinking and patient care abilities.
Frequently Asked Questions
1. How long does a typical Band 6 Nurse interview last?
A typical Band 6 Nurse interview usually lasts between 30 to 60 minutes. This duration allows the interviewers to assess both your clinical skills and personal attributes. Expect to answer questions about your nursing experience, teamwork, and how you handle challenging situations. Be prepared for potential scenario-based questions that evaluate your problem-solving abilities. Make sure to manage your time effectively during the interview to convey your skills and experiences succinctly.
2. What should I wear to a Band 6 Nurse interview?
For a Band 6 Nurse interview, it’s best to wear professional attire that reflects your seriousness about the position. Opt for business casual clothing, such as a smart blouse or shirt paired with tailored trousers or a knee-length skirt. Avoid overly casual attire like jeans or sneakers. Additionally, ensure your overall appearance is neat and tidy, as this demonstrates professionalism and respect for the interviewers and the healthcare environment.
3. How many rounds of interviews are typical for a Band 6 Nurse position?
Typically, a Band 6 Nurse position may involve one or two rounds of interviews. The first round often focuses on your qualifications and experiences, while the second may delve deeper into your clinical skills and fit within the team. Some organizations may also include practical assessments or scenario-based evaluations. It’s essential to prepare for both types of interviews to showcase your comprehensive nursing knowledge and interpersonal skills effectively.
4. Should I send a thank-you note after my Band 6 Nurse interview?
Yes, sending a thank-you note after your Band 6 Nurse interview is highly recommended. It demonstrates your appreciation for the opportunity and reinforces your interest in the position. In your note, briefly express gratitude for the interviewer’s time, mention something specific discussed during the interview, and reiterate your enthusiasm for the role. This small gesture can leave a positive impression and may set you apart from other candidates.