Preparing for a Clinical Governance interview is a crucial step for anyone aiming to excel in the healthcare sector. This role is unique as it combines clinical knowledge with managerial skills to ensure patient safety, quality of care, and adherence to regulations. Proper interview preparation allows candidates to demonstrate their understanding of clinical governance principles, risk management, and quality improvement initiatives. In this comprehensive guide, we will cover essential questions you might face, effective strategies to articulate your experiences, and insights into the competencies that interviewers look for in candidates. By the end, you’ll be well-equipped to showcase your suitability for this vital position in healthcare.
- What to Expect in a Clinical Governance Interview
- Clinical Governance Interview Questions For Freshers
- Clinical Governance Intermediate Interview Questions
- Clinical Governance Interview Questions for Experienced
- How to Prepare for Your Clinical Governance Interview
- Common Clinical Governance Interview Mistakes to Avoid
- Key Takeaways for Clinical Governance Interview Success
- Frequently Asked Questions
What to Expect in a Clinical Governance Interview
In a Clinical Governance interview, candidates can expect a combination of behavioral and situational questions aimed at assessing their understanding of patient safety, quality improvement, and regulatory compliance. Interviews may be conducted by a panel including healthcare managers, clinical directors, and quality assurance professionals. The structure typically begins with introductory questions about the candidate’s background, followed by in-depth discussions on relevant experiences and case studies. Candidates may also face scenario-based questions to evaluate their critical thinking and problem-solving skills in real-world clinical situations.
Clinical Governance Interview Questions For Freshers
Clinical Governance interview questions for freshers focus on essential concepts related to quality assurance, patient safety, and ethical practices in healthcare. Candidates should be familiar with the principles of clinical governance, risk management strategies, and ways to improve healthcare delivery.
1. What is Clinical Governance?
Clinical Governance is a systematic approach to maintaining and improving the quality of patient care within a health system. It encompasses a wide range of activities, including risk management, clinical audit, patient involvement, and continuous professional development. The goal is to ensure that healthcare providers deliver high-quality services while minimizing risks to patients.
2. Why is patient safety important in Clinical Governance?
Patient safety is a fundamental aspect of Clinical Governance because it ensures that healthcare services do not cause harm to patients. It involves identifying potential risks, implementing safety protocols, and fostering a culture of transparency and learning. Ensuring patient safety helps to improve trust in healthcare systems and enhances overall health outcomes.
3. What are some key components of Clinical Governance?
- Clinical Effectiveness: Ensuring that treatments and interventions are based on the best available evidence.
- Risk Management: Identifying, assessing, and mitigating risks to patient safety.
- Patient Involvement: Engaging patients in their care and decision-making processes.
- Education and Training: Continuous professional development for healthcare staff to improve skills and knowledge.
These components work together to create a safer healthcare environment and enhance the quality of care provided.
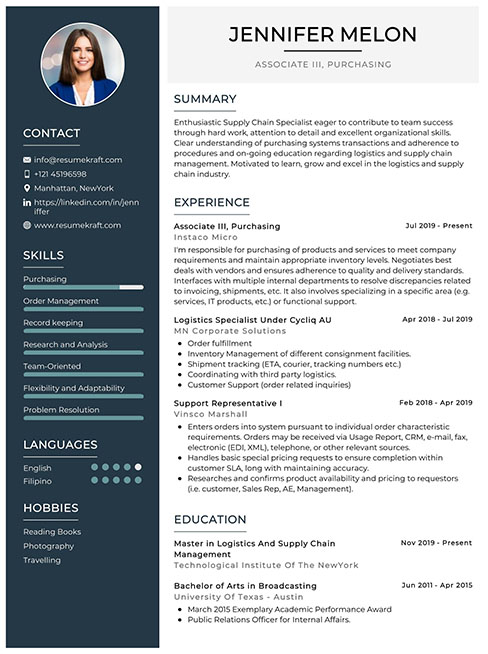
Build your resume in just 5 minutes with AI.
4. How does a clinical audit contribute to quality improvement?
A clinical audit is a systematic review of clinical performance against established standards. It helps identify areas for improvement by comparing current practices with best practices. By analyzing the results, healthcare organizations can implement changes that enhance care quality, ensure compliance with guidelines, and monitor progress over time.
5. What role does evidence-based practice play in Clinical Governance?
Evidence-based practice involves making clinical decisions based on the best available evidence, clinical expertise, and patient preferences. In Clinical Governance, it ensures that healthcare interventions are effective and safe, leading to improved patient outcomes. It also fosters a culture of continuous learning and adaptation in healthcare settings.
6. Can you explain what risk management entails in healthcare?
Risk management in healthcare involves identifying, assessing, and prioritizing risks, followed by coordinated efforts to minimize, monitor, and control the probability of unfortunate events. This includes analyzing incidents, implementing safety protocols, and engaging staff in training, thereby ensuring a safer environment for both patients and healthcare professionals.
7. What is the significance of patient feedback in Clinical Governance?
Patient feedback is crucial in Clinical Governance as it provides insights into patient experiences and satisfaction. It helps healthcare providers identify areas for improvement, enhance service delivery, and tailor care to meet patient needs. Incorporating feedback fosters a patient-centered approach, ultimately leading to better health outcomes.
8. Describe the concept of continuous professional development (CPD).
Continuous Professional Development (CPD) refers to ongoing learning and skill enhancement for healthcare professionals. It involves participation in educational activities, workshops, and training programs that keep professionals updated on the latest practices and research. CPD is critical for maintaining competency and improving the quality of care delivered to patients.
9. What is an adverse event, and how should it be handled?
An adverse event is an unintended injury or complication resulting from healthcare management rather than the underlying condition of the patient. It should be handled by promptly reporting the incident, conducting a thorough investigation, implementing corrective actions, and communicating transparently with affected patients. This process ensures learning from incidents to prevent future occurrences.
10. How can healthcare organizations foster a culture of safety?
- Encourage Open Communication: Create an environment where staff can report safety concerns without fear of retribution.
- Provide Training: Regularly train staff on safety protocols and incident reporting.
- Recognize and Reward Safe Practices: Acknowledge staff who contribute to safety improvements.
By implementing these strategies, organizations can enhance their safety culture and improve patient care quality.
11. What is the role of leadership in Clinical Governance?
Leadership plays a vital role in Clinical Governance by setting a clear vision for quality improvement, fostering a culture of safety, and ensuring accountability. Leaders are responsible for allocating resources, supporting staff training, and promoting a patient-centered approach, which collectively drives the organization towards better health outcomes.
12. Explain the term “patient involvement” in healthcare.
Patient involvement refers to engaging patients in their own healthcare decisions, encouraging them to participate actively in discussions about their treatment options and care plans. This approach respects patient preferences and values, leading to improved satisfaction, adherence to treatment, and ultimately better health outcomes.
13. What is the importance of clinical guidelines?
Clinical guidelines are systematically developed statements that assist healthcare providers in making decisions about appropriate healthcare for specific clinical circumstances. They are essential for standardizing care, ensuring evidence-based practices, and improving patient safety by guiding practitioners in providing consistent and high-quality treatment.
14. How does data analysis contribute to Clinical Governance?
Data analysis plays a crucial role in Clinical Governance by enabling healthcare organizations to track performance metrics, identify trends, and assess the effectiveness of interventions. Analyzing data helps organizations make informed decisions, improve patient outcomes, and ensure compliance with regulatory standards. It serves as a foundation for continuous quality improvement efforts.
15. What strategies can be employed to improve healthcare quality?
- Implementing Evidence-Based Practices: Ensuring care is guided by the best available research.
- Enhancing Communication: Fostering clear communication among healthcare teams and with patients.
- Conducting Regular Audits: Assessing compliance with standards and identifying areas for improvement.
These strategies can help organizations achieve higher quality care and foster a culture of excellence in healthcare delivery.
These questions are designed for freshers entering the Clinical Governance field and cover fundamental concepts they should master.
16. What is Clinical Governance?
Clinical Governance is a systematic approach to maintaining and improving the quality of patient care within a health system. It involves ensuring that healthcare professionals are accountable for their performance and that patients receive safe, effective, and high-quality care. The framework includes policies, procedures, and practices aimed at fostering a culture of continuous improvement in healthcare services.
17. Why is Clinical Governance important in healthcare?
Clinical Governance is crucial because it enhances patient safety and quality of care by establishing clear accountability among healthcare professionals. It promotes transparency, encourages continuous learning, and enables healthcare organizations to identify and mitigate risks. This leads to better patient outcomes, increased patient satisfaction, and fosters a culture of excellence within healthcare settings.
18. What are the key components of Clinical Governance?
- Clinical Effectiveness: Ensuring treatments are based on the best available evidence.
- Risk Management: Identifying and managing risks to ensure patient safety.
- Patient Involvement: Engaging patients in their own care and decision-making processes.
- Staff Management: Supporting and training staff to deliver high-quality care.
- Information Management: Collecting and analyzing data to improve services.
These components work together to create a comprehensive framework that supports the delivery of safe and effective care.
19. How does Clinical Governance support patient safety?
Clinical Governance supports patient safety by implementing systems that ensure care is delivered according to established guidelines and best practices. It includes regular audits, incident reporting, and feedback mechanisms that help identify areas for improvement. By fostering a culture of safety, healthcare organizations can proactively address issues before they affect patients.
20. What role does evidence-based practice play in Clinical Governance?
Evidence-based practice is a cornerstone of Clinical Governance, as it ensures that clinical decisions are made based on the best available evidence from research and clinical guidelines. This approach enhances the quality of care, reduces variability in treatment, and leads to improved patient outcomes by ensuring that healthcare providers utilize effective interventions.
21. Can you explain the significance of patient feedback in Clinical Governance?
Patient feedback is vital in Clinical Governance as it provides insights into the patient experience and highlights areas for improvement. By analyzing feedback, healthcare organizations can make informed decisions to enhance service delivery, address concerns, and tailor care to meet patient needs, ultimately leading to improved satisfaction and outcomes.
22. What is the role of audits in Clinical Governance?
Audits play a critical role in Clinical Governance by systematically reviewing clinical practices and outcomes to ensure compliance with established standards. They help identify gaps in care delivery, assess the effectiveness of interventions, and provide data that can be used to improve processes and outcomes, ensuring continuous quality improvement.
23. How can technology enhance Clinical Governance?
Technology enhances Clinical Governance by providing tools for data collection, analysis, and reporting. Electronic health records (EHRs) streamline information sharing and improve communication among healthcare providers. Data analytics can identify trends and measure performance, while telemedicine can facilitate patient engagement and access to care, thereby supporting better governance.
Clinical Governance Intermediate Interview Questions
Clinical Governance interview questions for intermediate candidates focus on essential concepts that ensure the delivery of high-quality healthcare. Candidates should understand frameworks for quality improvement, risk management, patient safety, and the role of clinical audits in enhancing service delivery.
24. What is Clinical Governance and why is it important?
Clinical Governance is a systematic approach to maintaining and improving the quality of patient care within a health system. It encompasses various components like risk management, quality improvement, and patient safety. It is crucial because it ensures accountability, enhances the standard of care, promotes a culture of continuous improvement, and ultimately leads to better patient outcomes.
25. Can you explain the role of clinical audits in Clinical Governance?
Clinical audits are systematic reviews of clinical performance against explicit criteria, aimed at improving patient care. They help identify areas for improvement by comparing current practices to established standards. The process includes collecting data, analyzing results, and implementing changes based on findings, which fosters a culture of accountability and continuous quality enhancement.
26. What is the significance of patient safety in Clinical Governance?
Patient safety is a core component of Clinical Governance, focusing on preventing harm to patients during healthcare delivery. It is significant because it fosters a culture where safety is prioritized, encourages reporting and learning from errors, and enhances patient trust in healthcare providers. Effective patient safety initiatives lead to improved health outcomes and reduce healthcare costs.
27. How do you implement a Quality Improvement (QI) initiative in a healthcare setting?
- Identify a specific area for improvement based on data analysis.
- Engage stakeholders and form a multidisciplinary team.
- Develop a clear plan with measurable goals and timelines.
- Implement changes using evidence-based practices.
- Monitor progress and adjust the plan as necessary based on feedback.
Effective implementation of QI initiatives requires ongoing communication, training, and a commitment to adapt based on results, fostering a culture of continuous improvement.
28. What are the key components of a risk management framework in healthcare?
- Risk Identification: Recognizing potential hazards that could cause harm.
- Risk Assessment: Evaluating the likelihood and impact of identified risks.
- Risk Control: Implementing measures to mitigate or eliminate risks.
- Monitoring and Review: Regularly reviewing risks and the effectiveness of control measures.
A robust risk management framework helps healthcare organizations minimize harm, enhance patient safety, and comply with regulatory requirements.
29. How do you measure the effectiveness of Clinical Governance initiatives?
The effectiveness of Clinical Governance initiatives can be measured through various metrics including patient outcomes, incident reporting rates, patient satisfaction surveys, and compliance with clinical guidelines. Regular audits and feedback mechanisms also play a critical role in assessing performance and identifying areas for further improvement.
30. What is the role of patient feedback in Clinical Governance?
Patient feedback is vital in Clinical Governance as it provides insights into patient experiences and satisfaction levels. It helps identify areas needing improvement, informs service delivery, and enhances patient-centered care. Incorporating patient feedback into decision-making processes promotes transparency and accountability, ultimately leading to better health outcomes.
31. Describe the concept of a “no blame culture” in healthcare.
A “no blame culture” in healthcare encourages open reporting of errors and near misses without fear of punishment. This approach promotes transparency, learning, and improvement rather than assigning blame. It fosters an environment where staff feel safe to discuss mistakes, leading to better patient safety and continuous quality improvement.
32. What are the potential challenges in implementing Clinical Governance?
- Resistance to Change: Staff may be hesitant to adopt new practices.
- Lack of Resources: Insufficient funding or personnel can hinder initiatives.
- Inadequate Training: Staff may not have the necessary skills or understanding of QI processes.
- Poor Communication: Ineffective communication can lead to misunderstandings and lack of engagement.
Addressing these challenges requires strong leadership, effective training programs, and a commitment to fostering a culture of improvement.
33. How can technology support Clinical Governance?
Technology can support Clinical Governance through electronic health records (EHRs), data analytics tools, and telemedicine. These technologies enable better data collection, facilitate clinical audits, enhance communication among healthcare teams, and improve patient engagement. By leveraging technology, healthcare organizations can streamline processes, enhance decision-making, and ultimately improve patient care.
34. What is the importance of interdisciplinary collaboration in Clinical Governance?
Interdisciplinary collaboration is crucial in Clinical Governance as it brings together diverse expertise and perspectives to address complex patient care issues. It fosters better communication, enhances problem-solving, and ensures comprehensive care planning. Collaborative efforts lead to more effective implementation of governance strategies, improving patient safety and quality of care.
35. How do you ensure compliance with clinical guidelines and standards?
- Regular Training: Provide ongoing education and training for staff on updated guidelines.
- Audits and Reviews: Conduct regular audits to evaluate compliance levels.
- Feedback Mechanisms: Create channels for staff to report challenges in adhering to guidelines.
- Leadership Support: Ensure strong leadership commitment to uphold clinical standards.
By implementing these strategies, organizations can maintain high standards of care and improve overall patient outcomes.
36. Describe a situation where you had to handle a clinical incident. What steps did you take?
In a previous role, I encountered a clinical incident where a medication error occurred. The steps I took included: immediately ensuring the patient’s safety, analyzing the cause of the error, notifying relevant stakeholders, documenting the incident, and conducting a root cause analysis. I also facilitated a debriefing session to discuss lessons learned and to implement corrective actions, ensuring that similar incidents would be prevented in the future.
37. What role does leadership play in Clinical Governance?
Leadership is essential in Clinical Governance as it sets the tone for a culture of quality and safety. Leaders are responsible for establishing governance frameworks, promoting accountability, supporting staff training, and ensuring resources are available for quality improvement initiatives. Effective leadership fosters an environment where staff are motivated to prioritize patient care and engage in continuous improvement efforts.
Here are some intermediate-level interview questions designed for candidates with knowledge of Clinical Governance. These questions focus on practical applications, best practices, and real-world scenarios within the field.
39. What is Clinical Governance and why is it important in healthcare?
Clinical Governance is a systematic approach to maintaining and improving the quality of patient care within a health system. It encompasses various components, including risk management, quality assurance, and patient safety. The importance of Clinical Governance lies in its ability to ensure that healthcare services are effective, safe, and patient-centered, thus enhancing the overall quality of care and fostering public trust in healthcare systems.
40. Can you describe the key components of Clinical Governance?
- Clinical Effectiveness: Ensuring treatments and interventions are based on the best available evidence.
- Risk Management: Identifying, assessing, and mitigating risks to patient safety.
- Patient Safety: Implementing strategies to prevent harm to patients during care delivery.
- Patient Experience: Focusing on the satisfaction and involvement of patients in their care.
- Staff Management: Supporting the ongoing training and development of healthcare professionals.
- Information Management: Using data to monitor performance and drive improvements.
These components work together to create a comprehensive framework that promotes high-quality care and continuous improvement in healthcare services.
41. How do you measure the effectiveness of Clinical Governance practices?
- Patient Outcomes: Tracking clinical outcomes to assess the impact of care delivered.
- Audit and Feedback: Performing regular audits and providing feedback to healthcare teams to identify areas for improvement.
- Patient Surveys: Conducting surveys to gather patient feedback on their experiences and satisfaction.
- Incident Reporting: Analyzing incident reports to identify trends and areas needing attention.
- Compliance with Standards: Evaluating adherence to clinical guidelines and regulatory requirements.
Measuring these factors allows organizations to assess the effectiveness of their Clinical Governance initiatives and make informed decisions for improvement.
42. What role does leadership play in Clinical Governance?
Leadership is crucial in Clinical Governance as it sets the tone for a culture of safety and quality within healthcare organizations. Leaders are responsible for establishing clear goals, promoting accountability, and ensuring that staff are engaged and empowered to contribute to quality improvement efforts. Effective leadership fosters an environment where open communication is encouraged, enabling staff to report concerns and share best practices without fear.
43. What are some common challenges in implementing Clinical Governance?
- Resistance to Change: Staff may be reluctant to adopt new processes or practices.
- Lack of Resources: Insufficient funding or staffing can hinder implementation efforts.
- Inadequate Training: Staff may not have the necessary training to effectively engage in Clinical Governance.
- Data Management: Difficulty in collecting and analyzing data can limit the ability to monitor progress.
- Fragmented Care: Coordination challenges among different departments can impede governance efforts.
Addressing these challenges is critical to successfully implementing Clinical Governance and ensuring high-quality care.
44. Explain how patient involvement is integrated into Clinical Governance.
Patient involvement is integrated into Clinical Governance through mechanisms that encourage patients to participate in their care and decision-making processes. This can include patient advisory councils, feedback surveys, and shared decision-making models. Engaging patients not only improves their satisfaction and outcomes but also provides valuable insights for healthcare providers, leading to more patient-centered care approaches and continuous quality improvement.
45. Describe a situation where Clinical Governance practices led to improved patient outcomes.
A notable example is a hospital that implemented a Clinical Governance framework focusing on reducing surgical site infections (SSIs). They adopted evidence-based practices, such as proper sterilization techniques, preoperative assessments, and postoperative care protocols. Following regular audits and staff training, the hospital saw a significant reduction in SSIs, leading to shorter hospital stays and improved patient satisfaction. This case exemplifies how Clinical Governance can lead to tangible improvements in patient outcomes.
46. What is the significance of incident reporting in Clinical Governance?
Incident reporting is vital in Clinical Governance as it serves as a primary tool for identifying and analyzing adverse events and near misses in healthcare settings. By encouraging staff to report incidents without fear of blame, organizations can gather data to understand the underlying causes of errors. This information is crucial for implementing preventive measures, enhancing safety protocols, and fostering a culture of continuous improvement, ultimately leading to better patient care.
Clinical Governance Interview Questions for Experienced
This section covers advanced Clinical Governance interview questions tailored for experienced professionals. These questions delve into topics such as system architecture, optimization strategies, scalability challenges, design patterns, and leadership in clinical settings, ensuring candidates can demonstrate their depth of knowledge and practical experience.
47. What is Clinical Governance and why is it essential in healthcare?
Clinical Governance is a systematic approach to maintaining and improving the quality of patient care within a health system. It emphasizes accountability, continuous improvement, and patient safety. It is essential because it ensures that healthcare services are effective, safe, and patient-centered, fostering a culture of transparency and accountability among healthcare professionals.
48. How do you implement a culture of continuous improvement within a clinical team?
Implementing a culture of continuous improvement involves several key strategies:
- Establishing clear goals: Define specific, measurable objectives for quality improvement.
- Encouraging feedback: Create an environment where team members feel comfortable sharing insights and suggestions.
- Training and education: Provide ongoing training to keep the team updated on best practices and new methodologies.
- Regular audits: Conduct audits and evaluations to identify areas for improvement and track progress.
This fosters a proactive approach to enhancing patient care and operational efficiency.
49. Can you describe a time when you led a quality improvement project?
In my previous role, I led a quality improvement project focused on reducing patient readmission rates. We analyzed data to identify high-risk patients and implemented a follow-up program that included telehealth check-ins. As a result, we reduced readmissions by 20% within six months, demonstrating effective collaboration and strategic planning.
50. What strategies do you use to ensure patient safety in clinical settings?
Ensuring patient safety involves a combination of proactive and reactive strategies:
- Implementing protocols: Establish clear clinical protocols and guidelines to minimize errors.
- Regular training: Conduct ongoing training sessions to keep staff informed about safety practices.
- Incident reporting systems: Encourage reporting of near misses and adverse events to learn from mistakes.
- Patient engagement: Involve patients in their care process to enhance adherence and safety.
These strategies create a safer environment for both patients and healthcare providers.
51. How do you assess the effectiveness of clinical governance initiatives?
Assessing the effectiveness of clinical governance initiatives can be achieved through the following methods:
- Key Performance Indicators (KPIs): Establish and monitor KPIs related to patient outcomes, safety incidents, and compliance with protocols.
- Patient feedback: Utilize surveys and feedback mechanisms to gauge patient satisfaction and experiences.
- Audit results: Conduct regular audits to evaluate adherence to clinical governance practices.
- Benchmarking: Compare performance with other healthcare organizations to identify areas for improvement.
This comprehensive approach provides insights into the success of initiatives and areas needing attention.
52. What role does data analytics play in clinical governance?
Data analytics plays a crucial role in clinical governance by enabling healthcare organizations to make informed decisions based on evidence. It helps in:
- Identifying trends: Analyzing patient outcomes and incidents to identify patterns and potential areas for improvement.
- Measuring performance: Evaluating the effectiveness of clinical practices and interventions through performance metrics.
- Resource allocation: Optimizing resource use by understanding where improvements can lead to better outcomes.
- Enhancing decision-making: Providing actionable insights that inform policy and clinical decisions.
These capabilities enhance the overall quality of care delivered to patients.
53. How do you handle conflicts within a clinical team?
Handling conflicts within a clinical team requires a structured approach:
- Active listening: Ensure all parties have the opportunity to express their views and concerns.
- Identifying common goals: Focus on shared objectives to foster collaboration.
- Facilitating open communication: Encourage discussions that promote understanding and resolution.
- Seeking mediation: If necessary, involve a neutral third party to help resolve the conflict.
This approach not only resolves conflicts but also strengthens team dynamics.
54. What are the key elements of an effective clinical audit?
An effective clinical audit should include the following key elements:
- Clear objectives: Define what the audit aims to achieve and the specific aspects of care being evaluated.
- Data collection: Gather accurate and relevant data to assess compliance with standards.
- Analysis: Analyze the data to identify trends, gaps, and areas for improvement.
- Action plan: Develop an action plan based on audit findings to implement necessary changes.
- Re-evaluation: Conduct follow-up audits to assess the impact of improvements made.
These elements ensure that the audit process contributes to enhanced patient care.
55. How do you foster a culture of accountability among staff?
Fostering a culture of accountability involves several strategies:
- Setting clear expectations: Clearly define roles and responsibilities for each team member.
- Providing feedback: Regularly give constructive feedback to reinforce positive behaviors and address areas for improvement.
- Encouraging ownership: Empower staff to take ownership of their work and decisions.
- Recognizing achievements: Celebrate individual and team successes to motivate continued accountability.
By implementing these strategies, accountability becomes ingrained in the organizational culture.
56. What are the challenges of implementing clinical governance in a large hospital?
Implementing clinical governance in a large hospital can present several challenges:
- Complexity of operations: The size and complexity of the organization can make it difficult to standardize practices across departments.
- Resistance to change: Staff may be resistant to new protocols or governance frameworks, impacting implementation.
- Resource limitations: Limited resources can hinder training, audits, and the implementation of new initiatives.
- Data integration: Integrating data from various departments for comprehensive analysis can be challenging.
Addressing these challenges requires strong leadership and a well-planned change management strategy.
57. How do you ensure compliance with regulatory standards in clinical governance?
Ensuring compliance with regulatory standards involves the following steps:
- Staying informed: Keep up-to-date with relevant regulations, guidelines, and best practices.
- Training staff: Provide regular training on compliance requirements and the importance of adherence.
- Conducting audits: Regularly audit clinical practices to identify compliance gaps and implement corrective actions.
- Engaging leadership: Involve leadership in compliance initiatives to emphasize its importance across the organization.
This proactive approach helps maintain high standards and reduces the risk of non-compliance.
58. What strategies do you use to improve patient engagement in clinical governance?
Improving patient engagement can be achieved through various strategies:
- Education: Provide patients with information about their conditions, treatment options, and the importance of clinical governance.
- Involvement in decision-making: Encourage patients to participate in decisions regarding their care.
- Feedback mechanisms: Implement systems for patients to share their experiences and suggestions.
- Transparency: Communicate openly about governance processes and how patient input affects care quality.
These strategies enhance the patient experience and promote a collaborative approach to healthcare.
59. How do you measure the success of clinical governance initiatives over time?
Measuring the success of clinical governance initiatives requires a multifaceted approach:
- Longitudinal studies: Conduct studies over time to assess changes in patient outcomes and safety metrics.
- Patient satisfaction surveys: Regularly collect data on patient satisfaction to gauge the impact of initiatives.
- Performance metrics: Track KPIs continuously to monitor improvements in clinical practice.
- Feedback loops: Establish mechanisms for ongoing feedback from staff and patients to refine initiatives.
This comprehensive measurement approach ensures that initiatives are effective and aligned with organizational goals.
60. What are your views on the role of technology in enhancing clinical governance?
Technology plays a pivotal role in enhancing clinical governance by:
- Improving data collection: Electronic health records and data analytics tools facilitate accurate and timely data collection.
- Enhancing communication: Communication platforms enable better collaboration among healthcare teams.
- Facilitating training: E-learning platforms provide accessible training for staff on governance practices and protocols.
- Monitoring compliance: Technology can automate compliance tracking and reporting, ensuring adherence to standards.
Overall, technology streamlines processes and improves the quality and safety of patient care.
These questions focus on advanced concepts in Clinical Governance, aimed at experienced professionals who are familiar with its complexities and implications in healthcare settings.
62. How would you implement a clinical governance framework in a healthcare organization?
Implementing a clinical governance framework involves several key steps:
- Assessment of Current Practices: Evaluate existing clinical practices and identify gaps in governance, quality, and safety.
- Stakeholder Engagement: Involve all relevant stakeholders, including healthcare professionals, management, and patients, to ensure comprehensive perspectives are considered.
- Policy Development: Create clear policies and procedures that outline the roles, responsibilities, and processes for maintaining clinical governance.
- Education and Training: Provide training for staff on the importance of clinical governance and how to adhere to the established framework.
- Monitoring and Evaluation: Establish mechanisms for ongoing monitoring, such as audits and feedback systems, to assess compliance and effectiveness of the framework.
Regular reviews and updates to the framework are crucial to adapt to changes in healthcare standards and practices.
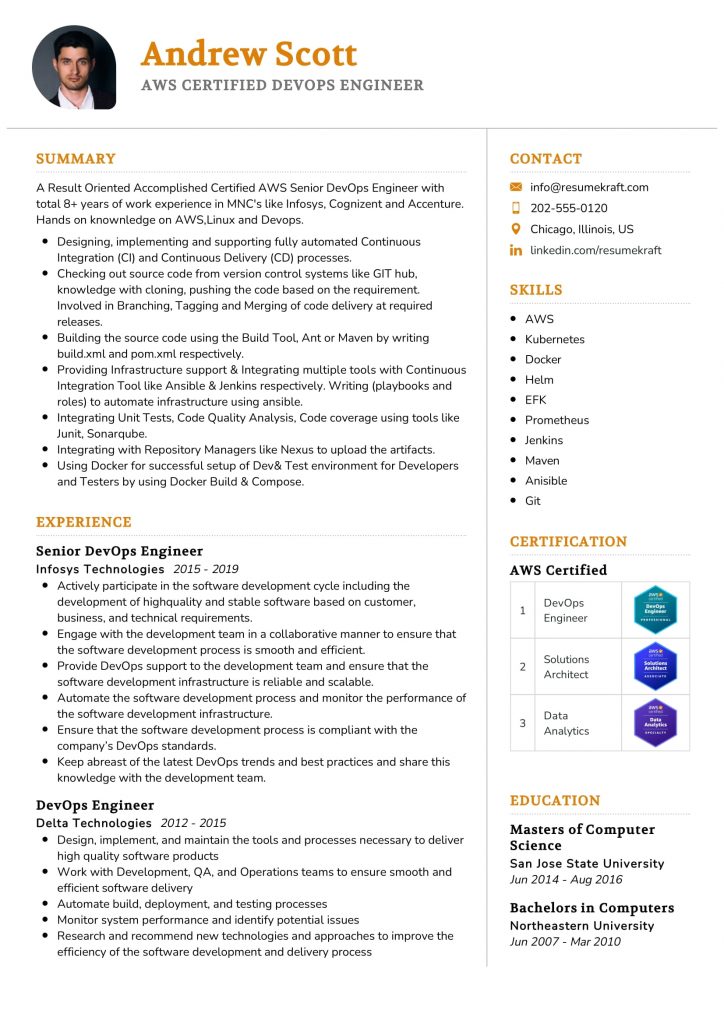
Build your resume in 5 minutes
Our resume builder is easy to use and will help you create a resume that is ATS-friendly and will stand out from the crowd.
63. What strategies would you use to foster a culture of safety and continuous improvement within a clinical governance framework?
Fostering a culture of safety and continuous improvement requires a multifaceted approach:
- Leadership Commitment: Leaders must demonstrate a commitment to safety by prioritizing it in policies and resource allocation.
- Open Communication: Encourage open dialogues about safety concerns without fear of retribution, allowing staff to share experiences and lessons learned.
- Training and Development: Regularly train staff on safety protocols, risk management, and quality improvement methods to enhance their skills.
- Patient Involvement: Engage patients in safety initiatives, such as feedback mechanisms, to understand their perspectives and improve care.
- Data-Driven Decisions: Utilize data analytics to track incidents and trends, enabling informed decision-making for safety improvements.
Ultimately, a culture of safety thrives on collaboration, transparency, and a commitment to learning from both successes and failures.
How to Prepare for Your Clinical Governance Interview
Preparing for a Clinical Governance interview requires a solid understanding of healthcare quality and safety standards. It’s essential to familiarize yourself with relevant regulations, frameworks, and best practices to demonstrate your knowledge and commitment to improving patient care and outcomes.
Review key legislation and frameworks related to clinical governance, such as the Care Quality Commission (CQC) guidelines and NHS frameworks. Understanding these regulations will help you articulate how they influence patient safety and quality improvement initiatives.
Familiarize yourself with common clinical governance tools and methodologies, such as root cause analysis, incident reporting systems, and clinical audits. Be prepared to discuss how you have used these in previous roles to enhance patient care and safety.
Reflect on your previous experiences in clinical governance or quality assurance roles. Prepare specific examples that showcase your skills, such as leading quality improvement projects or addressing safety concerns in a clinical setting.
Understand the principles of patient involvement and engagement in clinical governance. Be ready to discuss strategies for involving patients in decision-making processes and how this can improve service delivery and patient satisfaction.
Stay informed about current trends and challenges in healthcare, especially regarding clinical governance. Read relevant journals, articles, or reports to discuss contemporary issues, such as digital health, patient safety culture, and quality indicators.
Practice common interview questions related to clinical governance, such as those about handling complaints, implementing change, or working within multi-disciplinary teams. Articulate your answers clearly and confidently, demonstrating your problem-solving skills.
Network with professionals in the clinical governance field. Attend workshops, seminars, or webinars to build connections and gain insights into best practices. This networking can provide valuable information and boost your confidence during the interview.
Common Clinical Governance Interview Mistakes to Avoid
When interviewing for a Clinical Governance position, avoiding common mistakes can significantly enhance your chances of success. Being well-prepared and aware of potential pitfalls will help you present yourself as a knowledgeable and capable candidate.
- Lack of Understanding of Clinical Governance: Failing to demonstrate a clear understanding of clinical governance principles can raise doubts about your suitability. Familiarize yourself with key concepts, frameworks, and policies to articulate your knowledge effectively.
- Ignoring Relevant Experience: Not emphasizing your relevant experience can make you seem unqualified. Highlight specific roles and responsibilities that relate directly to clinical governance and showcase your contributions to improving patient safety and quality of care.
- Not Preparing for Behavioral Questions: Many interviews include behavioral questions to assess your problem-solving and leadership skills. Prepare specific examples demonstrating how you’ve tackled challenges in past roles related to clinical governance.
- Neglecting Current Trends and Regulations: Failing to discuss current trends or regulations in clinical governance can suggest that you are not keeping up with developments in the field. Stay informed about recent changes and be ready to discuss their implications.
- Inadequate Knowledge of the Organization: Not researching the organization can lead to missed opportunities to connect your experience with their specific needs. Understand their clinical governance framework and recent initiatives to align your responses.
- Poor Communication Skills: In clinical governance, clear communication is essential. Ensure you articulate your thoughts succinctly and confidently, avoiding jargon that could confuse your interviewers.
- Failing to Ask Insightful Questions: Not having questions prepared can indicate a lack of interest. Prepare thoughtful questions that reflect your understanding of the role and the organization’s approach to clinical governance.
- Not Demonstrating a Patient-Centric Approach: Neglecting to emphasize a patient-centered mindset can be detrimental. Highlight your commitment to improving patient outcomes and safety through effective governance strategies.
Key Takeaways for Clinical Governance Interview Success
- Prepare your resume meticulously using effective resume templates to ensure clarity and professionalism. An AI resume builder can assist in creating an impactful document that highlights your skills.
- Showcase your experience with relevant resume examples that align with the clinical governance role. Tailor your achievements to demonstrate your understanding of governance principles and practices.
- Craft compelling cover letters that reflect your passion for clinical governance. Personalize each letter to the organization, emphasizing how your values align with their mission and goals.
- Engage in mock interview practice to build confidence and improve your responses. Familiarize yourself with common clinical governance questions and refine your answers through continuous feedback.
- Research the organization’s clinical governance framework and recent initiatives. Having this knowledge will help you articulate how you can contribute effectively during the interview.
Frequently Asked Questions
1. How long does a typical Clinical Governance interview last?
A typical Clinical Governance interview lasts between 30 to 60 minutes. The duration can vary depending on the organization’s structure and the complexity of the role. During this time, you can expect to engage in discussions about your experience, competencies, and understanding of clinical governance principles. It’s advisable to prepare for a range of questions and be ready to elaborate on your past experiences, demonstrating how they relate to the role you are applying for.
2. What should I wear to a Clinical Governance interview?
For a Clinical Governance interview, it is best to dress in professional business attire. Men typically wear suits with a tie, while women may opt for suits or professional dresses. The goal is to convey professionalism and respect for the interview process. Ensure that your clothing is clean, well-fitted, and appropriate for a healthcare setting. Additionally, avoid overly casual attire or distracting accessories to maintain focus on your qualifications and interview performance.
3. How many rounds of interviews are typical for a Clinical Governance position?
Typically, a Clinical Governance position may involve two to three rounds of interviews. The first round often includes a preliminary screening, which may be conducted by HR or a hiring manager. Subsequent rounds usually involve more in-depth discussions with clinical leaders or panel interviews that assess your technical knowledge and fit within the organization. Being prepared for multiple rounds allows you to showcase your skills and adaptability throughout the interview process.
4. Should I send a thank-you note after my Clinical Governance interview?
Yes, sending a thank-you note after your Clinical Governance interview is highly recommended. It demonstrates your appreciation for the opportunity and reinforces your interest in the position. A brief, thoughtful message can differentiate you from other candidates, highlighting key points discussed during the interview. Aim to send the note within 24 hours, and personalize it by mentioning specific topics from the interview that resonated with you, further establishing a connection with the interviewers.