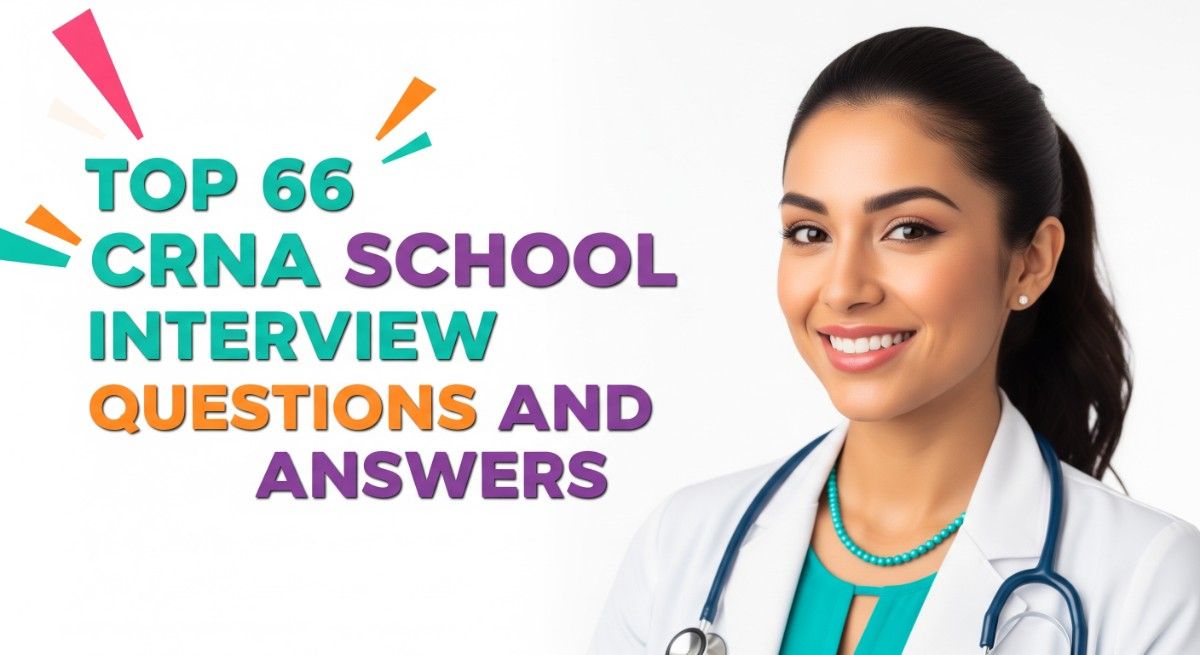
Preparing for a Certified Registered Nurse Anesthetist (CRNA) school interview is a pivotal step in advancing your nursing career. The role of a CRNA is unique, as it combines advanced clinical skills with critical thinking in high-stakes environments, requiring not only technical knowledge but also exceptional communication and interpersonal abilities. Proper interview preparation is essential to convey your passion and competence effectively, allowing you to stand out among candidates. This comprehensive guide will cover common interview questions, strategies for presenting your experiences, tips on building rapport with interviewers, and insights into what programs look for in potential CRNAs, ensuring you approach your interview with confidence and clarity.
What to Expect in a CRNA School Interview
In a CRNA school interview, candidates can expect a structured process involving multiple formats, including one-on-one interviews and panel interviews. Typically, the interviewers may consist of faculty members, practicing CRNAs, and occasionally, nurse anesthetist students. Candidates are often assessed on their clinical knowledge, critical thinking skills, and interpersonal abilities. The interview may include behavioral questions, scenario-based questions, and discussions about past experiences in healthcare. Additionally, candidates should be prepared to articulate their motivations for pursuing a career in anesthesia and demonstrate their commitment to the field.
CRNA School Interview Questions For Freshers
Preparing for CRNA School interviews is crucial for freshers aiming to enter the field of nurse anesthesia. Candidates should focus on mastering fundamental concepts such as pharmacology, anesthesia principles, patient assessment, and clinical skills to effectively demonstrate their knowledge and readiness for this advanced practice role.
1. What are the primary roles and responsibilities of a CRNA?
A Certified Registered Nurse Anesthetist (CRNA) is responsible for administering anesthesia and monitoring patients throughout surgical procedures. Their primary roles include conducting pre-anesthesia assessments, developing anesthesia care plans, administering anesthesia agents, monitoring patient vitals, and managing post-anesthesia care. CRNAs also collaborate with surgical teams to ensure patient safety and comfort.
2. Can you explain the different types of anesthesia?
- General Anesthesia: Induces unconsciousness and loss of sensation across the entire body, used for major surgeries.
- Regional Anesthesia: Blocks sensation in a specific area of the body, such as spinal or epidural anesthesia.
- Local Anesthesia: Numbs a small area of the body for minor procedures, allowing the patient to remain fully awake.
Understanding these types is essential for CRNAs to choose the appropriate technique based on the patient’s needs and the surgical procedure.
3. What is the importance of pharmacology in anesthesia?
Pharmacology is critical in anesthesia as it involves understanding the effects, interactions, and dosing of various anesthetic agents. CRNAs must be knowledgeable about the pharmacokinetics and pharmacodynamics of these drugs to ensure safe and effective anesthesia management. This knowledge aids in selecting the right agents, anticipating side effects, and managing potential complications during procedures.
Build your resume in just 5 minutes with AI.
4. How do you assess a patient before administering anesthesia?
Pre-anesthesia assessments involve reviewing the patient’s medical history, conducting a physical examination, and evaluating any relevant lab results. Key factors include the patient’s age, weight, allergies, existing medical conditions, and previous anesthesia experiences. This comprehensive assessment helps identify potential risks and tailor the anesthesia plan to optimize patient safety.
5. What are some common complications associated with anesthesia?
- Nausea and Vomiting: Common aftereffects, especially with general anesthesia.
- Respiratory Issues: Airway obstruction or hypoxia can occur, requiring immediate intervention.
- Cardiovascular Complications: Changes in heart rate or blood pressure can happen and must be monitored closely.
Being aware of these complications allows CRNAs to take proactive measures to mitigate risks during procedures.
6. Describe the process of intubation.
Intubation involves placing an endotracheal tube into a patient’s trachea to maintain an open airway during anesthesia. The process includes pre-oxygenation, administering anesthetic agents, and using a laryngoscope to visualize the vocal cords. The tube is then inserted, and proper placement is confirmed by auscultation and capnography. This skill is critical for managing patients’ airways effectively.
7. What is the role of monitoring during anesthesia?
Monitoring during anesthesia is vital to ensure patient safety and the effectiveness of the anesthetic technique. Key parameters include heart rate, blood pressure, oxygen saturation, and end-tidal CO2 levels. Continuous monitoring allows CRNAs to identify any adverse reactions or complications promptly and adjust anesthesia delivery as needed to maintain patient stability.
8. How do you handle patient allergies related to anesthesia?
Handling patient allergies involves a thorough review of the patient’s medical history to identify known allergies. If allergies to anesthetic agents are present, alternative medications or techniques are considered. During the procedure, the CRNA ensures that emergency protocols are in place to address any allergic reactions, including having epinephrine and other emergency medications readily available.
9. What are anesthetic agents, and how are they classified?
- Inhalational Agents: Gases administered through a mask or endotracheal tube, such as sevoflurane and isoflurane.
- Intravenous Agents: Drugs injected directly into the bloodstream, such as propofol and ketamine.
- Adjunct Medications: Used to enhance the effects of anesthetics, including opioids and muscle relaxants.
Understanding these classifications helps CRNAs select appropriate anesthetic strategies tailored to individual patient needs.
10. What is the significance of informed consent in anesthesia?
Informed consent is a critical ethical and legal requirement in anesthesia. It involves explaining the anesthesia plan, potential risks, benefits, and alternatives to the patient. Ensuring that the patient understands this information and agrees to proceed allows for shared decision-making and promotes trust between the patient and the healthcare team, ultimately enhancing patient care.
11. How do CRNAs manage pain in post-anesthesia care?
CRNAs manage post-anesthesia pain through various strategies, including the administration of analgesics, regional anesthesia techniques, and multimodal pain management approaches. They assess pain levels using standardized scales and adjust pain management plans accordingly. Effective pain control is essential for patient comfort and can significantly impact recovery outcomes.
12. Can you discuss the importance of teamwork in the operating room?
Teamwork in the operating room is crucial for ensuring patient safety and optimal outcomes. CRNAs work closely with surgeons, nurses, and other healthcare professionals to coordinate care. Effective communication, mutual respect, and collaboration enhance the surgical experience, minimize errors, and foster a supportive environment for both the patient and the surgical team.
13. What are the ethical considerations in anesthesia practice?
- Patient Autonomy: Respecting the patient’s right to make informed decisions about their care.
- Beneficence: Ensuring that the anesthesia care provided is in the best interest of the patient.
- Non-maleficence: Avoiding harm to patients by following best practices and standards of care.
Being aware of these ethical principles guides CRNAs in their clinical decision-making and enhances patient trust.
14. How do you stay current with advancements in anesthesia?
Staying current with advancements in anesthesia involves continuous education through attending professional conferences, participating in workshops, subscribing to relevant journals, and engaging in peer discussions. CRNAs must commit to lifelong learning to integrate new techniques, medications, and technologies into their practice, ensuring high-quality patient care and safety.
15. Why do you want to become a CRNA?
Many candidates express a desire to become a CRNA due to the combination of advanced practice, autonomy, and the opportunity to make a significant impact on patient care. The role allows for a deep connection with patients during critical moments, and many find the challenge and complexity of anesthesia to be intellectually rewarding, further fueling their passion for the profession.
These questions are designed for freshers entering CRNA School and cover fundamental concepts and skills essential for success in the field.
16. What is the primary role of a Certified Registered Nurse Anesthetist (CRNA)?
The primary role of a CRNA is to administer anesthesia and provide anesthesia care for patients undergoing surgical or medical procedures. CRNAs assess patients’ medical histories, develop anesthesia care plans, monitor patients throughout procedures, and ensure their safety and comfort before, during, and after anesthesia. They work independently or as part of a healthcare team, often in various settings such as hospitals, surgical centers, and pain management clinics.
17. What are the different types of anesthesia that CRNAs can administer?
- General Anesthesia: Induces a state of unconsciousness and loss of sensation throughout the body.
- Regional Anesthesia: Blocks sensation in a specific area of the body, such as an epidural or spinal anesthesia.
- Local Anesthesia: Numbs a small area of the body for minor procedures without affecting consciousness.
- Monitored Anesthesia Care (MAC): Provides sedation and analgesia while allowing the patient to remain responsive.
Understanding these types of anesthesia is crucial for CRNAs to tailor their approach based on the patient’s needs and the surgical procedure.
18. How do CRNAs evaluate a patient’s suitability for anesthesia?
CRNAs evaluate a patient’s suitability for anesthesia through a thorough pre-anesthesia assessment that includes reviewing the patient’s medical history, conducting a physical examination, and assessing any laboratory results. They consider factors such as allergies, current medications, past anesthesia experiences, and existing medical conditions. This comprehensive evaluation helps in formulating an individualized anesthesia plan and identifying any potential risks or complications.
19. What are some common complications that can arise from anesthesia?
- Nausea and Vomiting: Common after general anesthesia, it can be managed with medications.
- Respiratory Issues: Difficulty in breathing or airway obstruction can occur, requiring prompt intervention.
- Cardiovascular Events: These can include changes in heart rate or blood pressure that must be monitored closely.
- Allergic Reactions: An adverse reaction to anesthetic agents, which can range from mild to severe.
Recognizing these potential complications is essential for CRNAs to ensure patient safety and to provide effective management strategies during and after anesthesia.
20. What monitoring techniques are used during anesthesia?
- Electrocardiogram (ECG): Monitors heart rate and rhythm.
- Pulse Oximetry: Measures oxygen saturation in the blood to ensure adequate oxygenation.
- Blood Pressure Monitoring: Important for assessing hemodynamic stability throughout the procedure.
- Capnography: Measures the concentration of carbon dioxide in exhaled air, indicating ventilation status.
These monitoring techniques are critical for maintaining patient safety and making real-time adjustments to the anesthesia plan as needed.
21. How does a CRNA handle an emergency situation during anesthesia?
In an emergency situation, a CRNA follows established protocols to ensure patient safety. This includes quickly assessing the situation, providing immediate care, and implementing appropriate interventions, such as airway management, administering medications, or calling for assistance. CRNAs are trained to remain calm under pressure, prioritize tasks, and utilize teamwork to effectively manage the emergency while maintaining patient stability.
22. Can you explain the importance of pharmacology in anesthesia practice?
Pharmacology is essential in anesthesia practice as it involves understanding the effects, interactions, and potential side effects of anesthetic agents and adjunct medications. CRNAs must be knowledgeable about drug dosages, routes of administration, and how various medications influence physiological responses. This knowledge is crucial for making informed decisions about anesthesia management and ensuring safe and effective patient care.
23. What role does patient communication play in the CRNA’s responsibilities?
Patient communication is vital in a CRNA’s responsibilities as it helps build trust, alleviate anxiety, and ensure that patients are informed about the anesthesia process. CRNAs must effectively explain the anesthesia plan, address any concerns, and obtain informed consent. Good communication fosters a collaborative environment and enhances patient satisfaction, which is essential for successful outcomes in anesthesia care.
CRNA School Intermediate Interview Questions
CRNA School interviews assess candidates on their understanding of advanced anesthesia concepts, patient care, and critical thinking skills. Intermediate-level candidates should be well-versed in pharmacology, anesthesia techniques, and the management of complex clinical scenarios to demonstrate their readiness for graduate-level training.
25. What are the most common anesthetic agents used in practice?
The most common anesthetic agents include Propofol, Sevoflurane, and Isoflurane. Propofol is favored for its rapid onset and recovery, making it ideal for outpatient procedures. Sevoflurane and Isoflurane are inhalational agents often used for maintenance anesthesia due to their favorable side effect profiles and quick elimination from the body.
26. How do you assess a patient’s airway before anesthesia?
Airway assessment involves several key components: evaluating the patient’s history for previous airway issues, observing the patient’s neck and jaw structure, and using the Mallampati classification to predict intubation difficulty. Additionally, assessing the range of motion of the neck and the presence of any obstructive conditions is important in planning airway management.
27. What is the significance of the ASA physical status classification system?
The ASA (American Society of Anesthesiologists) classification system evaluates a patient’s pre-anesthesia medical status. It ranges from ASA I (healthy) to ASA VI (declared brain-dead). This classification helps anesthetists gauge the risk of anesthesia and surgery, guiding decision-making for perioperative management and patient safety.
28. Explain the concept of pharmacokinetics and pharmacodynamics in anesthesia.
- Pharmacokinetics: Refers to how the body absorbs, distributes, metabolizes, and excretes anesthetic drugs. Understanding these processes helps predict drug levels in the bloodstream and their effects over time.
- Pharmacodynamics: Describes the effects of drugs on the body, including the mechanisms of action and the relationship between drug concentration and effect. This knowledge is crucial for dosing and managing potential side effects.
Understanding both pharmacokinetics and pharmacodynamics is essential for safe and effective anesthesia management.
29. What are the potential complications of regional anesthesia?
- Neurological complications: These can include nerve damage, transient neurological symptoms, or prolonged weakness.
- Infection: There is a risk of infection at the site of injection, which can lead to serious complications.
- Vascular complications: Accidental injection into a blood vessel can lead to systemic toxicity.
Awareness of these complications allows for better risk management and patient safety during procedures.
30. Describe the role of intraoperative monitoring during anesthesia.
Intraoperative monitoring is critical for ensuring patient safety during anesthesia. It typically includes monitoring vital signs such as heart rate, blood pressure, oxygen saturation, and end-tidal carbon dioxide. Advanced monitoring may include neuromuscular function and depth of anesthesia. These data help anesthetists adjust anesthetic levels and manage potential complications in real-time.
31. What is the purpose of preoperative assessment in anesthesia?
The preoperative assessment aims to identify any potential risks or complications related to anesthesia and surgery. It involves reviewing the patient’s medical history, performing a physical examination, and ordering necessary tests. This assessment helps formulate an anesthesia plan tailored to the patient, ensuring optimal safety and outcomes during the surgical procedure.
32. How do you manage a patient experiencing hypotension during surgery?
- Assess the cause: Determine if hypotension is due to anesthesia, blood loss, or other factors.
- Administer fluids: Administer IV fluids to expand intravascular volume, if appropriate.
- Use vasopressors: Medications like ephedrine or phenylephrine can help raise blood pressure if fluid resuscitation is insufficient.
Prompt recognition and appropriate management of hypotension are crucial for maintaining hemodynamic stability during surgery.
33. What are the criteria for extubation after anesthesia?
- Awake and alert: The patient should be awake, able to follow commands, and demonstrate adequate respiratory effort.
- Stable vital signs: Consistent and stable heart rate, blood pressure, and oxygen saturation levels must be present.
- Effective airway reflexes: The patient should show signs of protective airway reflexes, such as coughing and swallowing.
Meeting these criteria helps ensure patient safety and minimizes the risk of airway complications postoperatively.
34. Discuss the importance of informed consent in anesthesia.
Informed consent is a fundamental ethical and legal requirement in anesthesia. It ensures that patients understand the risks, benefits, and alternatives to the anesthesia plan, allowing them to make informed decisions about their care. This process promotes transparency, fosters trust between the patient and healthcare provider, and minimizes liability issues for practitioners.
35. What are the signs of malignant hyperthermia, and how should it be managed?
- Signs: Symptoms include a rapid increase in body temperature, muscle rigidity, tachycardia, and metabolic acidosis.
- Management: Immediate cessation of triggering agents, administration of dantrolene sodium, and supportive measures like cooling the patient and managing acidosis are critical.
Recognizing and managing malignant hyperthermia is vital for patient safety during anesthesia.
36. Explain the differences between local anesthesia and general anesthesia.
- Local anesthesia: Blocks sensation in a specific area of the body without affecting consciousness. It is used for minor procedures.
- General anesthesia: Induces a state of unconsciousness and loss of sensation throughout the entire body, used for major surgeries.
Choosing between local and general anesthesia depends on the type of procedure, patient factors, and the desired level of comfort.
37. What is the significance of the capnography monitoring during anesthesia?
Capnography measures the concentration of carbon dioxide in exhaled air and provides real-time feedback on a patient’s ventilation status. It helps detect hypoventilation, airway obstruction, or equipment malfunction. Continuous monitoring of capnography is essential for assessing the effectiveness of ventilation and ensuring patient safety during anesthesia.
38. How would you approach pain management in a postoperative patient?
- Assessment: Evaluate the patient’s pain level using a standardized scale to determine appropriate interventions.
- Multimodal approach: Implement a combination of medications (opioids, non-opioids, adjuvants) and non-pharmacological methods (ice, relaxation techniques) for optimal pain control.
- Continuous reassessment: Monitor the patient’s response to pain management and adjust the plan as necessary.
A comprehensive pain management strategy enhances patient comfort and promotes quicker recovery.
These questions are designed for candidates preparing for a Certified Registered Nurse Anesthetist (CRNA) school interview, focusing on clinical knowledge, critical thinking, and practical applications in anesthesia care.
40. What are the key differences between general anesthesia and regional anesthesia?
General anesthesia involves rendering a patient completely unconscious and unresponsive to stimuli, often using inhaled gases and intravenous agents. In contrast, regional anesthesia blocks sensation in a specific area of the body, allowing the patient to remain awake or sedated while feeling is eliminated in the targeted region. This approach is often used for procedures on the limbs or lower body and typically results in fewer systemic side effects compared to general anesthesia.
41. How do you assess a patient’s airway before anesthesia?
- Visual Inspection: Examine the patient’s facial structure, neck length, and any signs of obesity or previous surgeries that may indicate potential airway issues.
- Modified Mallampati Classification: This classification system assesses the visibility of the oropharyngeal structures to predict the difficulty of intubation.
- Thyromental Distance: Measure the distance from the thyroid notch to the mentum; a shorter distance may indicate a difficult airway.
Proper assessment is crucial for planning anesthesia management and anticipating challenges during intubation.
42. What factors can affect the pharmacokinetics of anesthetic agents?
- Age: Older patients may have altered drug metabolism and clearance due to decreased organ function.
- Weight: Obesity can affect the volume of distribution and drug potency, necessitating adjustments in dosing.
- Comorbidities: Conditions such as liver or kidney disease can significantly impact drug metabolism and elimination.
Understanding these factors helps in tailoring anesthetic plans to achieve optimal outcomes and minimize complications.
43. Can you explain the role of the CRNA in preoperative assessment?
The CRNA plays a crucial role in the preoperative assessment by evaluating the patient’s medical history, performing physical examinations, and conducting a thorough airway assessment. They also review relevant laboratory and diagnostic tests, discuss anesthesia options with the patient, and address any concerns. This process helps identify potential risks and formulates an individualized anesthesia plan, enhancing patient safety and comfort.
44. Describe the importance of monitoring during anesthesia.
- Patient Safety: Continuous monitoring of vital signs ensures that any changes can be detected and addressed promptly.
- Assessment of Anesthetic Depth: Monitoring helps determine the appropriate depth of anesthesia to prevent awareness during surgery.
- Detection of Complications: Monitoring can reveal signs of hemodynamic instability or adverse reactions to anesthetic agents.
Effective monitoring throughout the procedure is vital to maintain a stable anesthetic condition and ensure patient safety.
45. What is the significance of a pre-anesthetic medication regimen?
A pre-anesthetic medication regimen is significant as it helps to reduce anxiety, manage pain, and minimize the risk of potential complications during anesthesia. Medications such as benzodiazepines can help calm patients, while opioids may provide analgesia. Additionally, premedication can facilitate smoother induction and emergence from anesthesia, leading to improved patient satisfaction and recovery experiences.
46. How would you handle a patient experiencing a severe allergic reaction during anesthesia?
In the event of a severe allergic reaction, immediate intervention is critical. The first step is to stop the administration of any suspected allergens. Administer oxygen to the patient and initiate IV access if not already established. Epinephrine should be given promptly to counteract anaphylaxis, followed by corticosteroids and antihistamines as needed. Continuous monitoring of vital signs and airway management is essential until the reaction is resolved.
47. What are the common complications associated with regional anesthesia?
- Nerve Injury: Accidental damage to nerves can result in temporary or permanent deficits.
- Hematoma Formation: This can occur if a blood vessel is punctured during the procedure, leading to bleeding in the epidural or subarachnoid space.
- Infection: There is a risk of infection at the injection site, which can lead to serious complications.
Understanding these complications allows CRNAs to take preventive measures and manage them effectively should they arise.
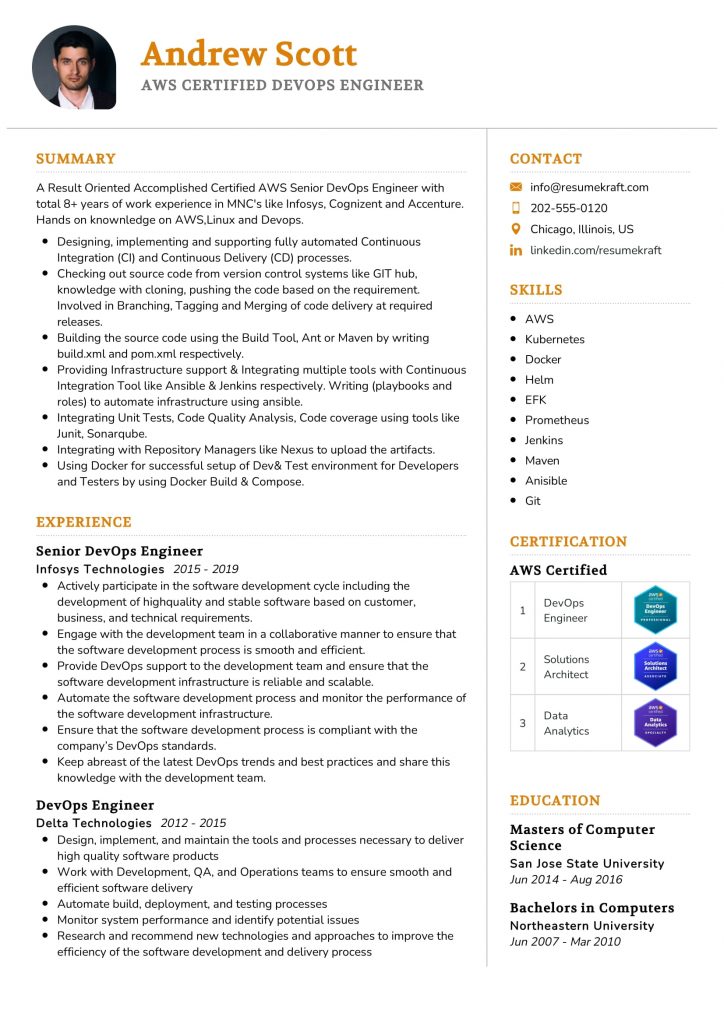
Build your resume in 5 minutes
Our resume builder is easy to use and will help you create a resume that is ATS-friendly and will stand out from the crowd.
48. What is the role of a CRNA in postoperative care?
The CRNA’s role in postoperative care includes monitoring the patient’s recovery from anesthesia, assessing vital signs, and managing pain control through appropriate analgesic techniques. They may also address any complications, such as nausea or respiratory issues, and provide education on postoperative care. This continuous oversight ensures a smooth transition from the operating room to recovery, promoting patient safety and comfort.
CRNA School Interview Questions for Experienced
This section focuses on CRNA School interview questions designed for experienced professionals. These questions delve into advanced topics such as anesthesia techniques, pharmacology, patient management, leadership in clinical settings, and the application of evidence-based practices in anesthesia care.
49. What are the key considerations for patient safety during anesthesia administration?
Patient safety during anesthesia administration is paramount and involves several key considerations: ensuring proper patient assessment, monitoring vital signs continuously, using appropriate anesthetic agents tailored to the patient’s health status, and having emergency protocols in place. Furthermore, effective communication among the surgical team and adherence to established protocols can significantly mitigate risks during procedures.
50. How do you approach a complex case with multiple comorbidities?
In a complex case with multiple comorbidities, I adopt a systematic approach: first, I conduct a thorough preoperative assessment to evaluate the patient’s medical history and current health status. Next, I collaborate with the surgical team to develop a tailored anesthesia plan that addresses each comorbidity. Continuous intraoperative monitoring and adjustments to the anesthesia plan based on real-time data are crucial to ensure patient safety and optimal outcomes.
51. Can you explain the concept of pharmacodynamics as it relates to anesthesia?
Pharmacodynamics refers to the effects of drugs on the body, particularly how anesthetic agents interact with receptors and affect physiological processes. Understanding pharmacodynamics is essential for CRNAs to predict drug actions, tailor anesthetic plans, and manage patient responses effectively. For instance, knowing the dose-response relationship allows for precise titration of anesthetics to achieve desired levels of sedation and analgesia.
52. What is your experience with different anesthesia techniques in special populations?
- Neonates and pediatrics: I adjust dosages and prefer regional anesthesia to minimize systemic effects.
- Geriatric patients: I focus on minimizing polypharmacy and using lighter anesthesia to reduce postoperative delirium.
- Patients with obesity: I utilize specialized airway management techniques and consider pharmacokinetics adjustments due to altered body composition.
Each population presents unique challenges that require tailored approaches to ensure safety and effectiveness.
53. Describe how you would handle a sudden intraoperative crisis.
In the event of a sudden intraoperative crisis, I would first assess the situation quickly to identify the cause, ensuring patient stability. I would then activate the emergency response team, communicate clearly with the surgical team about the issue, and implement established protocols. Continuous monitoring of the patient’s vital signs is critical. Finally, I would document the event thoroughly to review and learn from the experience afterward.
54. What role does evidence-based practice play in your anesthesia practice?
Evidence-based practice is integral to my anesthesia practice as it involves integrating clinical expertise with the best available research evidence. By staying updated on the latest studies and guidelines, I can provide the safest and most effective anesthesia care. This practice also encourages critical thinking and continuous improvement in patient outcomes, as I apply proven techniques and protocols tailored to individual patient needs.
55. How do you ensure effective communication with the surgical team?
Effective communication with the surgical team is achieved through preoperative briefings, clear role definitions, and regular updates during the procedure. I prioritize active listening and encourage team members to voice concerns or observations. Utilizing standardized communication tools, such as SBAR (Situation, Background, Assessment, Recommendation), enhances clarity and reduces the risk of misunderstandings, ultimately improving patient safety.
56. Can you discuss the importance of mentorship in anesthesia?
Mentorship in anesthesia is crucial for fostering professional development and ensuring high standards of care. Experienced CRNAs can provide guidance on complex case management, share best practices, and support the growth of less experienced practitioners. A strong mentorship relationship encourages knowledge transfer, builds confidence in clinical skills, and promotes a culture of continuous learning within the anesthesia community.
57. What strategies do you use for pain management in the postoperative period?
- Multimodal analgesia: I use a combination of opioids and non-opioid medications to enhance pain relief while minimizing side effects.
- Regional anesthesia techniques: I often employ nerve blocks to provide targeted pain control.
- Patient education: I ensure patients are aware of pain management plans and encourage them to communicate their pain levels effectively.
These strategies help optimize patient comfort and recovery outcomes.
58. How do you approach quality assurance in your practice?
Quality assurance in my practice involves regular monitoring of clinical outcomes, participation in peer reviews, and adherence to established guidelines. I also engage in continuous education and training to stay current with best practices. Feedback from patient experiences is invaluable and is used to identify areas for improvement. Implementing changes based on data-driven insights ensures high-quality anesthesia care.
59. Explain the role of simulation training in anesthesia education.
Simulation training plays a critical role in anesthesia education by providing a safe environment for practitioners to practice technical skills and decision-making without risking patient safety. Through realistic scenarios, CRNAs can enhance their clinical judgment, refine their responses to emergencies, and improve teamwork. This hands-on experience is invaluable for building confidence and competence in managing complex clinical situations.
60. What is your experience with research in the field of anesthesia?
My experience with research in anesthesia includes participating in clinical trials, conducting retrospective studies, and presenting findings at conferences. I focus on areas such as optimizing anesthesia techniques for specific populations and evaluating the effectiveness of new medications. Engaging in research enhances my understanding of evidence-based practices and contributes to the advancement of anesthesia knowledge and patient care standards.
61. How do you assess and manage anesthesia-related complications?
Assessing and managing anesthesia-related complications requires vigilant monitoring and rapid response. I begin by identifying signs of complications, such as hypotension or airway obstruction. Immediate actions are taken based on the nature of the complication, such as administering fluids for hypotension or securing the airway. Post-event, I conduct a thorough review of the incident to develop strategies that prevent future occurrences.
62. Describe how you incorporate technology into your anesthesia practice.
Incorporating technology into my anesthesia practice involves utilizing advanced monitoring systems, electronic health records, and anesthesia delivery systems. These technologies enhance patient monitoring, streamline documentation, and improve communication within the surgical team. I also leverage simulation tools for training and skill development. Embracing technology not only enhances patient safety but also optimizes workflow efficiency.
These questions are designed for candidates applying to CRNA (Certified Registered Nurse Anesthetist) schools, focusing on advanced practice nursing, anesthesia principles, and patient care. They assess both technical knowledge and leadership qualities.
64. How do you ensure the safe administration of anesthesia in a clinical setting?
Ensuring the safe administration of anesthesia involves several critical steps: conducting a thorough pre-anesthetic assessment to identify any risk factors, utilizing appropriate monitoring equipment throughout the procedure, and adhering to established protocols for drug administration. Continuous communication with the surgical team and vigilant monitoring of the patient’s vital signs are essential. Moreover, being prepared for emergencies with a clear plan and immediate access to necessary medications and equipment is crucial for patient safety.
65. Can you describe a time when you had to mentor a colleague in anesthesia practices? What approach did you take?
In mentoring a colleague, I employed a hands-on approach combined with reflective learning. I first assessed their current knowledge and skill level, then provided tailored clinical practice opportunities. Utilizing a buddy system, I guided them through various procedures, encouraging questions and discussions. Additionally, I shared relevant literature and resources to deepen their understanding. This method not only enhanced their practical skills but also fostered confidence in their decision-making abilities.
66. What design patterns do you find most useful in developing protocols for anesthesia care?
- Singleton Pattern: This pattern ensures that a class has only one instance and provides a global point of access. In anesthesia protocols, it can be used for centralizing drug inventory management systems.
- Observer Pattern: Useful for monitoring patient responses during anesthesia, where various components can observe and react to changes in the patient’s status, ensuring timely interventions.
These design patterns aid in creating efficient and scalable systems in clinical practice, improving both patient care and operational efficiency.
How to Prepare for Your CRNA School Interview
Preparing for a CRNA School interview requires thorough planning and practice. Focus on understanding the role, demonstrating your clinical expertise, and showcasing your passion for anesthesia. Here are seven actionable tips to help you excel in your interview.
- Research the Program: Familiarize yourself with the specific CRNA program’s values, faculty, and curriculum. Understanding their unique offerings will allow you to tailor your responses and show genuine interest in their training philosophy.
- Review Clinical Knowledge: Brush up on anesthesia principles, pharmacology, and patient assessment skills. Be prepared to discuss how you would handle various clinical scenarios, demonstrating your critical thinking and decision-making abilities in high-pressure situations.
- Practice Common Interview Questions: Anticipate questions like “Why do you want to become a CRNA?” or “Describe a challenging clinical experience.” Practice your answers out loud to build confidence and ensure your responses are clear and concise.
- Prepare Your Own Questions: Formulate thoughtful questions to ask the interviewers about the program, clinical placements, or research opportunities. This shows your engagement and helps you assess if the school aligns with your career goals.
- Highlight Teamwork and Leadership: Discuss your experiences in collaborative healthcare settings and any leadership roles you’ve held. CRNAs often work closely with healthcare teams, so showcasing your ability to lead and collaborate is essential.
- Dress Professionally: Choose attire that reflects professionalism appropriate for a healthcare setting. Dressing well can boost your confidence and create a positive first impression, reinforcing your seriousness about the program.
- Follow Up: After the interview, send a thank-you email to your interviewers expressing gratitude for the opportunity. This not only demonstrates professionalism but also keeps you on their radar as a candidate who values communication and relationships.
Common CRNA School Interview Mistakes to Avoid
When interviewing for a Certified Registered Nurse Anesthetist (CRNA) School position, candidates often make critical mistakes that can hinder their chances of acceptance. Understanding these common pitfalls can help you present yourself as a strong candidate.
- Inadequate Preparation: Failing to research the program or its faculty can signal a lack of genuine interest. Candidates should familiarize themselves with the school’s mission, values, and specific curriculum details to engage effectively during the interview.
- Weak Understanding of Anesthesia: Not being able to articulate basic anesthesia concepts can indicate a lack of commitment. Candidates should review fundamental topics and recent advancements in the field to demonstrate their knowledge and enthusiasm.
- Poor Communication Skills: Inability to convey thoughts clearly can leave a negative impression. Candidates should practice articulating their experiences and motivations to ensure they present their qualifications confidently and coherently.
- Neglecting to Ask Questions: Not preparing insightful questions for the interviewers can suggest disinterest. Candidates should develop thoughtful questions that reflect their curiosity about the program and their future role as CRNAs.
- Overemphasis on Experience: Focusing too much on past experiences without relating them to the CRNA role can be misguided. Candidates should connect their clinical experiences to how they inform their understanding of anesthesia and patient care.
- Negative Attitude: Speaking poorly about previous employers or experiences can raise red flags. Candidates should maintain a positive demeanor and focus on lessons learned from past challenges, showcasing resilience and professionalism.
- Ignoring Non-Verbal Cues: Poor body language or lack of eye contact can convey disinterest or insecurity. Candidates should practice maintaining good posture, eye contact, and active listening to convey confidence and engagement.
- Failing to Follow Up: Not sending a thank-you note post-interview can be seen as a lack of professionalism. Candidates should express gratitude to their interviewers, reinforcing their interest in the program and leaving a positive impression.
Key Takeaways for CRNA School Interview Success
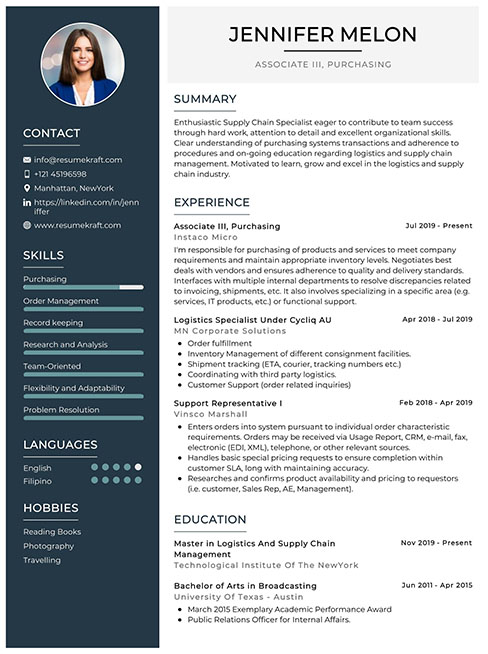
- Prepare a polished resume using effective resume templates. Consider utilizing an AI resume builder to ensure your qualifications are presented clearly and professionally.
- Showcase your experience with strong resume examples that highlight relevant clinical skills and educational background, ensuring you align your qualifications with the CRNA program’s expectations.
- Craft tailored cover letters that express your passion for anesthesia and your commitment to the CRNA profession, demonstrating how your background fits the program’s values.
- Engage in mock interview practice to refine your responses and boost your confidence. This will help you articulate your motivations and experiences effectively during the actual interview.
- Research common interview questions specific to CRNA schools and prepare thoughtful answers that reflect your understanding of the role and the challenges faced in the field.
Frequently Asked Questions
1. How long does a typical CRNA School interview last?
A typical CRNA School interview lasts between 30 minutes to 1 hour. This duration allows the interviewers to assess your clinical knowledge, motivation for the profession, and interpersonal skills. It’s important to prepare to discuss your experiences, answer behavioral questions, and demonstrate your understanding of the nurse anesthesia field. Being concise yet thorough in your responses will help you make the most of the time allotted and leave a positive impression on the interviewers.
2. What should I wear to a CRNA School interview?
For a CRNA School interview, it’s best to dress professionally. A well-fitted suit in a neutral color, such as navy or gray, is appropriate for both men and women. Women may opt for a tailored dress or a blouse with dress pants or a skirt. Ensure your attire is clean, pressed, and conservative. Additionally, pay attention to grooming and accessories, as a polished appearance reflects your seriousness about the program and professionalism in the nursing field.
3. How many rounds of interviews are typical for a CRNA School position?
Typically, CRNA Schools conduct one or two rounds of interviews. The first round often includes a panel interview with faculty and possibly current students, focusing on your clinical experiences and motivations. If you progress, a second interview may be more in-depth and could involve additional faculty members or a one-on-one format. Preparing for both types is essential, as each round assesses different aspects of your candidacy and fit for the program.
4. Should I send a thank-you note after my CRNA School interview?
Yes, sending a thank-you note after your CRNA School interview is highly recommended. It shows your appreciation for the opportunity and reinforces your interest in the program. Aim to send a personalized note within 24-48 hours of the interview, expressing gratitude for the interviewers’ time and highlighting a key point discussed. This gesture can leave a positive impression and keep you fresh in their minds as they make their decisions.