Preparing for a Pharmacology interview is an exciting yet challenging journey, as this role is pivotal in the healthcare sector. Pharmacologists play a crucial part in drug development, ensuring safety and efficacy while navigating complex regulatory environments. Proper interview preparation is essential, as it not only helps you showcase your technical knowledge but also your ability to communicate effectively and collaborate within interdisciplinary teams. This comprehensive guide will cover key interview questions, essential pharmacological concepts, and strategies to demonstrate your expertise and passion for the field. With the right preparation, you’ll be well-equipped to impress your interviewers and secure your place in this vital profession.
What to Expect in a Pharmacology Interview
In a Pharmacology interview, candidates can expect a mix of technical and behavioral questions designed to assess their knowledge of drug mechanisms, pharmacokinetics, and pharmacodynamics. Interviews may be conducted by a panel that includes pharmacists, clinical researchers, or hiring managers from pharmaceutical companies. The structure typically includes an introduction, followed by questions about relevant experience and technical expertise, and may conclude with a discussion on the candidate’s problem-solving abilities and teamwork skills. Candidates may also face case studies or scenario-based questions to evaluate their practical application of pharmacological principles.
Pharmacology Interview Questions For Freshers
This set of interview questions for freshers in pharmacology focuses on fundamental concepts essential for a strong foundation in the field. Candidates should master topics such as drug classifications, mechanisms of action, pharmacokinetics, and pharmacodynamics to excel in their interviews.
1. What is pharmacology?
Pharmacology is the branch of medicine and biology that studies the interactions between drugs and living organisms. It encompasses the understanding of how drugs affect biological systems, their therapeutic effects, side effects, and mechanisms of action. Pharmacologists aim to develop drugs that maximize therapeutic benefits while minimizing adverse effects.
2. What are the main branches of pharmacology?
- Pharmacodynamics: This branch studies the effects of drugs on biological systems and their mechanisms of action.
- Pharmacokinetics: It focuses on how the body absorbs, distributes, metabolizes, and excretes drugs.
- Clinical Pharmacology: This involves the study of drugs in humans, focusing on their efficacy and safety in clinical settings.
- Toxicology: This branch deals with the harmful effects of drugs and chemicals on living organisms.
Understanding these branches helps pharmacologists develop new medications and improve existing ones.
3. What is the difference between efficacy and potency?
Efficacy refers to the maximum effect a drug can produce, regardless of the dose. Potency, on the other hand, indicates the amount of drug needed to achieve a specific effect. A drug can be highly potent (requiring a small dose) but less efficacious compared to another drug that requires a larger dose to achieve a higher maximum effect.
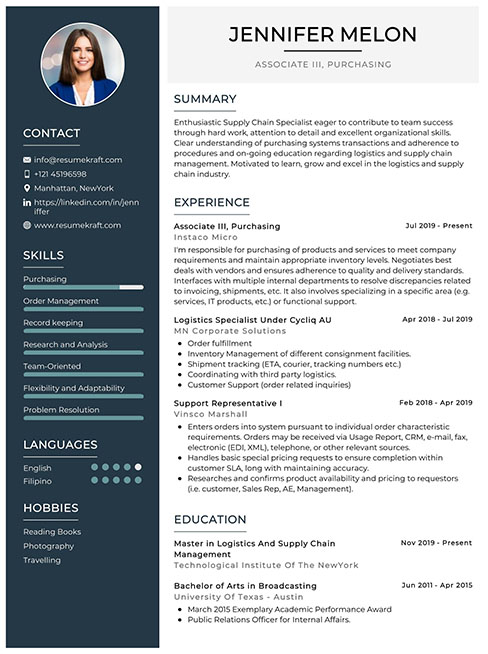
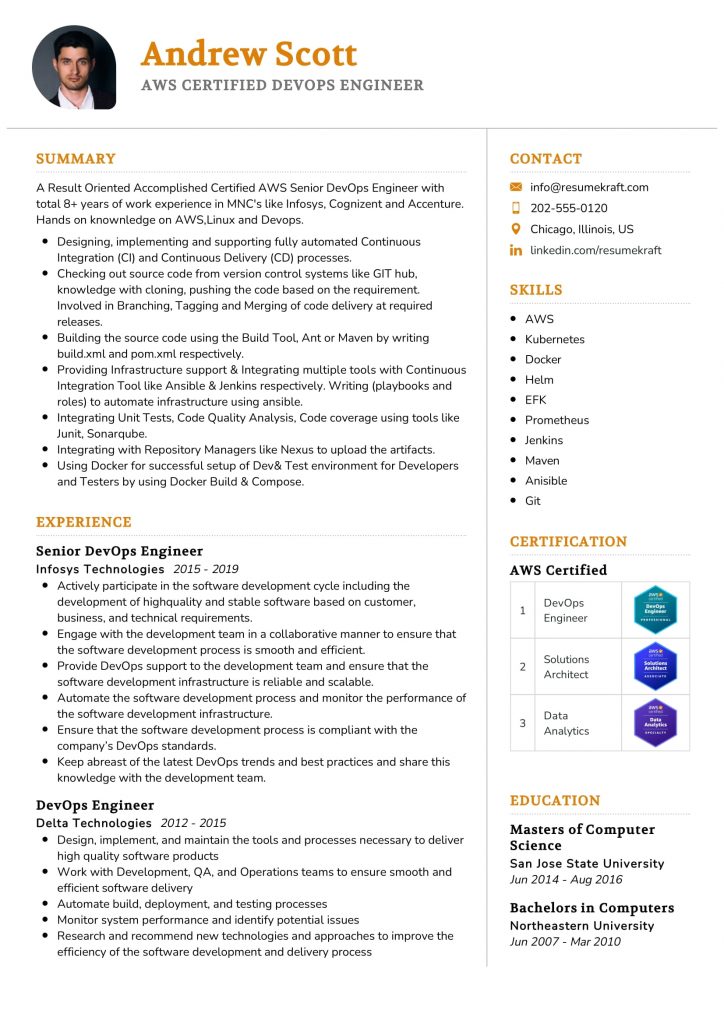
Build your resume in just 5 minutes with AI.
4. Explain the concept of half-life in pharmacology.
The half-life of a drug is the time it takes for the concentration of the drug in the bloodstream to reduce to half its initial value. It is a crucial parameter in pharmacokinetics, influencing dosing schedules and the duration of drug action. Understanding half-life helps in predicting how long a drug will remain effective and when to administer subsequent doses.
5. What are the different routes of drug administration?
- Oral: Drugs are taken by mouth and absorbed through the digestive system.
- Intravenous: Drugs are injected directly into the bloodstream for rapid effect.
- Intramuscular: Drugs are injected into muscle tissue for slower absorption.
- Subcutaneous: Drugs are injected under the skin for gradual absorption.
- Topical: Drugs are applied directly to the skin or mucous membranes.
Each route has its advantages and disadvantages, affecting the onset, intensity, and duration of drug action.
6. What is the significance of the therapeutic index?
The therapeutic index is a measure of a drug’s safety, defined as the ratio between the toxic dose and the effective dose. A high therapeutic index indicates a wider safety margin, meaning the drug is less likely to cause adverse effects at therapeutic doses. Conversely, a low therapeutic index suggests a higher risk of toxicity, requiring careful monitoring during treatment.
7. Define adverse drug reactions (ADRs).
Adverse drug reactions are unintended and harmful responses to medications administered at normal doses. ADRs can range from mild side effects to severe, life-threatening conditions. Understanding ADRs is vital for ensuring patient safety and effective treatment, as they can impact medication compliance and overall patient outcomes.
8. What role do enzymes play in pharmacology?
Enzymes play a critical role in drug metabolism, influencing how quickly drugs are processed and eliminated from the body. They can activate prodrugs into their active forms or facilitate the breakdown of active drugs into inactive metabolites. Enzyme activity can vary among individuals, affecting drug efficacy and safety due to genetic differences or interactions with other substances.
9. Explain the term ‘bioavailability.’
Bioavailability refers to the proportion of a drug that enters the systemic circulation when administered and is available for therapeutic action. It is influenced by the route of administration, formulation, and individual patient factors. Understanding bioavailability is essential for determining appropriate dosing regimens and ensuring effective drug therapy.
10. What is pharmacogenomics?
Pharmacogenomics is the study of how an individual’s genetic makeup affects their response to drugs. This field aims to tailor drug therapy based on genetic variations, optimizing efficacy and minimizing adverse effects. By understanding pharmacogenomic factors, healthcare providers can make informed decisions about drug selection and dosing for personalized medicine.
11. Describe the process of drug discovery and development.
The drug discovery and development process involves several stages:
- Target identification: Identifying biological molecules that are involved in disease processes.
- Lead compound identification: Discovering and optimizing compounds that interact with the identified targets.
- Preclinical testing: Evaluating the safety and efficacy of lead compounds in laboratory and animal studies.
- Clinical trials: Conducting human studies to assess safety, efficacy, and dosage.
- Regulatory approval: Submitting data to regulatory agencies for approval before market release.
This process is lengthy and complex, often taking years to ensure a drug is safe and effective for public use.
12. What is the significance of clinical trials?
Clinical trials are essential for determining the safety and efficacy of new drugs in humans before they can be approved for general use. They involve several phases, each designed to answer specific questions about the drug’s effects, optimal dosing, and potential side effects. The results from clinical trials inform regulatory decisions and guide clinical practice.
13. Explain the concept of tolerance in pharmacology.
Tolerance occurs when a person’s response to a drug diminishes over time, requiring larger doses to achieve the same effect. This can happen due to physiological adaptations or changes in drug metabolism. Understanding tolerance is crucial for managing long-term medication use and preventing withdrawal symptoms or overdose.
14. What are the common classifications of drugs?
- Analgesics: Medications used to relieve pain.
- Antibiotics: Drugs that fight bacterial infections.
- Antidepressants: Medications used to treat depression and anxiety disorders.
- Antihypertensives: Drugs that help lower blood pressure.
- Anticoagulants: Medications that prevent blood clotting.
Understanding these classifications aids in recognizing the therapeutic use of various drugs and their mechanisms of action.
15. What is the role of the FDA in drug approval?
The FDA (Food and Drug Administration) is responsible for ensuring the safety, efficacy, and security of drugs, biological products, and medical devices. Before a new drug can be marketed, it must undergo rigorous testing and review by the FDA, which assesses clinical trial data to determine whether the benefits of a drug outweigh its risks. The FDA also monitors post-marketing safety and can take action if new risks are identified.
These questions are designed for freshers entering the Pharmacology field and cover fundamental concepts they should master.
16. What is pharmacology?
Pharmacology is the branch of medicine and biology that studies the effects of drugs on biological systems. It involves understanding how drugs interact with the body, their mechanisms of action, therapeutic effects, and potential side effects. Pharmacologists study the chemical properties of drugs, their metabolism, and how they can be used to treat various diseases and conditions. This field bridges the gap between medical science and therapeutic practice.
17. What are the different phases of drug development?
- Discovery and Development: Involves identifying potential drug candidates and conducting preclinical testing to assess safety and efficacy.
- Clinical Trials: This phase is divided into three stages (Phase I to III) where the drug is tested on humans for safety, dosing, and efficacy.
- Regulatory Review: After successful trials, the drug is submitted for approval to regulatory agencies such as the FDA.
- Post-Marketing Surveillance: After approval, the drug’s long-term effects are monitored in the general population.
Each phase is critical in ensuring that the drug is safe and effective for public use, contributing to informed prescribing and patient care.
18. Explain the concept of bioavailability.
Bioavailability refers to the proportion of a drug or active ingredient that enters the systemic circulation when introduced into the body and is available for therapeutic effect. It is a crucial pharmacokinetic parameter because it affects the efficacy of the drug. Factors influencing bioavailability include the drug’s formulation, route of administration, and individual patient factors such as metabolism and absorption rates.
19. What are the routes of drug administration?
- Oral: Drugs are taken by mouth and absorbed through the gastrointestinal tract.
- Intravenous (IV): Drugs are injected directly into the bloodstream for immediate effect.
- Intramuscular (IM): Drugs are injected into a muscle, allowing for slower absorption.
- Subcutaneous (SC): Drugs are injected into the tissue layer between the skin and muscle.
- Topical: Drugs are applied directly to the skin or mucous membranes.
Each route has its advantages and disadvantages and is chosen based on the drug’s properties and desired effect.
20. What is the difference between agonists and antagonists?
Agonists are substances that activate receptors to produce a biological response, mimicking the action of a naturally occurring substance. For example, morphine is an agonist that binds to opioid receptors, producing pain relief. In contrast, antagonists inhibit the action of agonists by blocking the receptor sites, preventing the natural substance from exerting its effect. An example of an antagonist is naloxone, which blocks opioid receptors and reverses opioid overdose.
Pharmacology Intermediate Interview Questions
This set of intermediate Pharmacology interview questions is designed for candidates who have a foundational understanding and are ready to delve deeper into essential pharmacological concepts. Candidates should be familiar with drug mechanisms, pharmacokinetics, pharmacodynamics, and clinical applications.
21. What is the difference between pharmacokinetics and pharmacodynamics?
Pharmacokinetics refers to how the body affects a drug, encompassing the processes of absorption, distribution, metabolism, and excretion (ADME). In contrast, pharmacodynamics focuses on how the drug affects the body, including the mechanisms of action and the relationship between drug concentration and effect. Understanding both concepts is essential for optimizing drug therapy.
22. How do you determine the therapeutic index of a drug?
The therapeutic index (TI) is determined by dividing the toxic dose by the effective dose of a drug. It is calculated using the formula: TI = TD50 / ED50, where TD50 is the dose that produces toxicity in 50% of the population, and ED50 is the dose that produces the desired therapeutic effect in 50% of the population. A higher TI indicates a safer drug.
23. What factors can influence drug absorption?
- Formulation: The form in which a drug is administered (tablet, liquid) can affect its absorption rate.
- Route of administration: Intravenous administration leads to immediate absorption, while oral routes may involve delays.
- Physiological conditions: pH, blood flow, and the presence of food can significantly influence absorption.
- Drug interactions: Certain medications can enhance or inhibit the absorption of others.
Understanding these factors helps in designing effective drug regimens.
24. What is first-pass metabolism, and why is it important?
First-pass metabolism refers to the process where a drug is metabolized in the liver before it reaches systemic circulation. This can significantly reduce the bioavailability of the drug. It is important because it helps determine the appropriate dosing of orally administered medications, ensuring effective therapeutic levels are achieved in the bloodstream.
25. Explain the concept of drug half-life.
The half-life of a drug is the time required for the concentration of the drug in the bloodstream to reduce by half. It is a crucial parameter that affects dosing frequency and duration of action. Drugs with short half-lives may require more frequent dosing, while those with long half-lives can be administered less often.
26. What are the common mechanisms of drug action?
- Agonism: Drugs that activate receptors to produce a biological response.
- Antagonism: Drugs that block receptors and inhibit biological responses.
- Enzyme inhibition: Drugs that inhibit enzymes to decrease or stop metabolic reactions.
- Transporter modulation: Drugs that affect the transport of substances across cell membranes.
Understanding these mechanisms is vital for drug development and therapeutic strategies.
27. What is the significance of the blood-brain barrier in pharmacology?
The blood-brain barrier (BBB) is a selective permeability barrier that protects the brain from potentially harmful substances while allowing essential nutrients to pass. Its significance in pharmacology lies in its impact on drug delivery; drugs intended for central nervous system actions must be able to cross the BBB, which poses a challenge in drug design.
28. How do you assess a patient’s response to a medication?
Assessing a patient’s response to medication involves several steps, including monitoring therapeutic outcomes, evaluating side effects, and conducting follow-up assessments. Clinicians may utilize clinical scales, laboratory tests, and patient feedback to determine medication efficacy and tolerability, thereby ensuring optimal treatment and necessary adjustments.
29. What are the implications of drug-drug interactions?
- Increased toxicity: One drug may enhance the toxicity of another, leading to adverse effects.
- Reduced efficacy: Concomitant use of drugs can decrease the therapeutic effectiveness of one or both agents.
- Altered pharmacokinetics: Interactions can affect absorption, metabolism, and excretion rates of drugs.
Understanding these interactions is essential for safe prescribing and patient management.
30. Describe the role of pharmacogenomics in personalized medicine.
Pharmacogenomics studies how genetic variations affect individual responses to drugs. This field plays a critical role in personalized medicine by allowing healthcare providers to tailor drug therapies based on a patient’s genetic makeup, thereby maximizing efficacy and minimizing adverse effects. This approach enhances treatment outcomes and promotes safer medication use.
31. What is the significance of clinical trials in drug development?
Clinical trials are crucial for evaluating the safety and efficacy of new drugs before they can be approved for public use. These trials provide systematic data on the drug’s effects, optimal dosages, and potential side effects across different populations. The rigorous testing ensures that only effective and safe medications reach the market.
32. Explain the concept of tolerance in pharmacology.
Tolerance refers to a phenomenon where the body becomes less responsive to a drug after prolonged use, requiring higher doses to achieve the same effect. This can occur due to physiological adaptations that alter drug metabolism or receptor sensitivity. Understanding tolerance is important for managing long-term drug therapies and preventing withdrawal symptoms.
33. What are the common routes of drug administration and their advantages?
- Oral: Convenient and safe for patients, suitable for self-administration.
- Intravenous: Provides immediate effects and allows for precise control over drug levels.
- Intramuscular: Allows for slower absorption and is useful for depot formulations.
- Topical: Minimizes systemic side effects and targets local tissues directly.
Each route has specific indications based on the drug’s properties and the desired therapeutic effect.
34. What is the role of the FDA in drug approval?
The Food and Drug Administration (FDA) plays a vital role in ensuring that drugs are safe and effective for public use. It regulates the approval process for new drugs, requiring extensive clinical trial data to assess safety, efficacy, and manufacturing quality. The FDA also monitors post-market drug safety and can mandate label changes or recalls if necessary.
Here are five intermediate-level interview questions for Pharmacology that cover practical applications and important concepts in the field.
36. What are the primary mechanisms of drug action?
Drugs act through various mechanisms, primarily including:
- Receptor binding: Drugs bind to specific receptors, triggering a physiological response.
- Enzyme inhibition: Some drugs inhibit enzymes, reducing the production of certain substances in the body.
- Ion channel modulation: Drugs can affect the opening or closing of ion channels, altering cell excitability.
- Transporter interaction: Some drugs block or enhance transporter proteins that regulate the movement of substances across cell membranes.
Understanding these mechanisms helps in predicting drug effects and interactions.
37. Explain the concept of bioavailability and its significance in pharmacology.
Bioavailability refers to the proportion of a drug that enters systemic circulation when introduced into the body and is available for therapeutic effect. It is crucial because:
- It determines the correct dosage: Different routes of administration (oral, intravenous, etc.) have varying bioavailability.
- It influences drug efficacy: Higher bioavailability can enhance the drug’s effectiveness and therapeutic outcomes.
- It impacts drug formulation: Understanding bioavailability helps in designing formulations for optimal absorption.
Monitoring bioavailability is essential for effective drug therapy and individualized patient care.
38. What factors can affect drug metabolism in the body?
Drug metabolism can be influenced by several factors, including:
- Genetic variations: Polymorphisms in metabolizing enzymes can lead to differences in drug clearance rates among individuals.
- Age: Metabolic capacity can decrease with age, affecting drug dosing and efficacy.
- Liver function: Liver diseases can impair metabolic pathways, necessitating dose adjustments.
- Drug interactions: Co-administration of other drugs can induce or inhibit metabolic enzymes, altering drug levels.
Recognizing these factors is important for optimizing therapeutic regimens and minimizing adverse effects.
39. Describe the role of pharmacokinetics in drug therapy.
Pharmacokinetics involves the study of how the body absorbs, distributes, metabolizes, and excretes drugs. Its role in drug therapy includes:
- Dosing regimens: Pharmacokinetic data help determine optimal dosing intervals and amounts.
- Therapeutic monitoring: Understanding how drugs behave in the body allows for monitoring plasma concentrations to avoid toxicity.
- Individualization of therapy: Pharmacokinetics aids in tailoring treatments based on patient-specific factors such as age, weight, and organ function.
Effective pharmacokinetic analysis is vital for achieving desired therapeutic outcomes and enhancing patient safety.
40. What is the significance of the therapeutic index in drug development?
The therapeutic index (TI) is a measure of a drug’s safety margin, defined as the ratio of the toxic dose to the therapeutic dose. Its significance includes:
- Safety assessment: A higher TI indicates a safer drug, while a lower TI requires careful monitoring and dosing.
- Guiding clinical use: Understanding TI helps clinicians make informed decisions regarding drug selection and patient management.
- Informing drug development: A favorable TI is a key consideration during the drug development process, influencing the likelihood of regulatory approval.
A clear understanding of the therapeutic index is essential for optimizing drug therapy and ensuring patient safety.
Pharmacology Interview Questions for Experienced
Pharmacology interview questions for experienced professionals delve into advanced topics such as drug interactions, pharmacokinetics, pharmacodynamics, therapeutic drug monitoring, and regulatory considerations. Candidates should be prepared to discuss their expertise in optimizing drug therapy, understanding complex biological systems, and mentoring junior staff in pharmacological practices.
41. What are the key differences between pharmacokinetics and pharmacodynamics?
Pharmacokinetics refers to the study of how the body absorbs, distributes, metabolizes, and excretes drugs, essentially focusing on the drug’s journey through the body. In contrast, pharmacodynamics examines the biochemical and physiological effects of drugs and their mechanisms of action on the body. Understanding both is crucial for optimizing therapeutic outcomes.
42. How do you approach drug-drug interactions in a clinical setting?
When assessing drug-drug interactions, I follow a systematic approach:
- Review the patient’s medication history to identify potential interactions.
- Consult drug interaction databases to evaluate the severity and clinical significance of the interactions.
- Adjust dosages or recommend alternative therapies as necessary to mitigate risks.
This process ensures patient safety and effective therapy management.
43. Can you explain the concept of therapeutic drug monitoring (TDM)?
Therapeutic drug monitoring (TDM) involves measuring drug concentrations in a patient’s bloodstream to optimize dosing regimens. This practice is particularly important for drugs with narrow therapeutic windows, where the difference between effective and toxic doses is small. TDM helps tailor therapy to individual patient needs, improving efficacy and reducing adverse effects.
Build your resume in 5 minutes
Our resume builder is easy to use and will help you create a resume that is ATS-friendly and will stand out from the crowd.
44. Describe the role of pharmacogenomics in personalized medicine.
Pharmacogenomics studies how an individual’s genetic makeup affects their response to drugs. This field plays a pivotal role in personalized medicine by allowing healthcare providers to tailor drug therapies based on genetic profiles. By identifying specific genetic variations, clinicians can predict drug efficacy and toxicity, ultimately improving treatment outcomes and minimizing adverse effects.
Build your resume in 5 minutes
Our resume builder is easy to use and will help you create a resume that is ATS-friendly and will stand out from the crowd.
45. What strategies do you use to optimize drug therapy in patients with comorbidities?
Optimizing drug therapy in patients with comorbidities involves several strategies:
- Conducting thorough assessments of all medications to identify potential interactions and duplications.
- Collaborating with interdisciplinary teams to create integrated treatment plans.
- Monitoring patient outcomes closely and adjusting therapies based on clinical responses.
This comprehensive approach ensures safe and effective management of complex patients.
46. How do you ensure compliance with regulatory guidelines in pharmacotherapy?
Ensuring compliance with regulatory guidelines involves:
- Staying updated on current laws, regulations, and guidelines from bodies such as the FDA and EMA.
- Implementing standard operating procedures (SOPs) for drug management processes.
- Conducting regular training sessions for staff to reinforce compliance practices.
This proactive approach minimizes risks and enhances patient safety.
47. Discuss the importance of dosage form selection in drug therapy.
Dosage form selection is crucial in pharmacotherapy as it directly affects drug absorption, distribution, and overall therapeutic efficacy. Factors to consider include:
- Patient-specific factors such as age, ability to swallow, and preferences.
- Drug characteristics including stability, solubility, and release properties.
- Therapeutic objectives, such as the need for immediate versus sustained release.
Careful selection can enhance patient adherence and treatment success.
48. What are the challenges you face in drug formulation development?
Challenges in drug formulation development include:
- Ensuring stability and compatibility of active ingredients and excipients.
- Addressing the unique pharmacokinetic properties of the drug.
- Regulatory compliance and meeting market demands.
Navigating these challenges requires a multidisciplinary approach and innovative problem-solving skills.
49. How do you mentor junior staff in pharmacology?
Mentoring junior staff involves:
- Providing structured training sessions on essential pharmacological concepts.
- Encouraging hands-on experience through shadowing and supervised practice.
- Offering regular feedback and fostering an open environment for questions.
This approach not only builds their knowledge base but also enhances their confidence in clinical decision-making.
50. Explain the concept of drug half-life and its clinical significance.
Drug half-life is the time required for the plasma concentration of a drug to reduce by half. It is clinically significant because it influences:
- Dosing intervals and frequency to maintain therapeutic levels.
- Duration of action and potential for accumulation in the body.
- Timing for monitoring drug levels in TDM.
Understanding half-life is essential for effective drug management.
51. What factors influence drug absorption in the body?
Drug absorption is influenced by several factors:
- Physicochemical properties of the drug, such as solubility and permeability.
- Route of administration, which affects the absorption rate.
- Presence of food or other substances in the gastrointestinal tract.
- Patient-specific factors, including age, health status, and genetic variations.
These factors must be considered when designing effective drug therapies.
52. Discuss the role of the blood-brain barrier in pharmacology.
The blood-brain barrier (BBB) is a selective permeable barrier that protects the brain from harmful substances while allowing essential nutrients to pass. Its role in pharmacology is significant because:
- It challenges the delivery of drugs intended to treat central nervous system disorders.
- Understanding its mechanisms can lead to the development of strategies for drug delivery across the BBB.
Research on the BBB is crucial for advancing treatments for neurological conditions.
53. How do you evaluate the efficacy of a new drug?
Evaluating the efficacy of a new drug involves a multi-faceted approach:
- Reviewing data from preclinical studies and clinical trials, focusing on endpoints such as symptom relief and side effects.
- Comparing outcomes with existing therapies to determine relative benefit.
- Conducting post-marketing surveillance to monitor long-term effects and effectiveness in diverse populations.
This comprehensive evaluation ensures informed decisions regarding drug approval and use.
54. What is the mechanism of action of ACE inhibitors?
ACE inhibitors work by inhibiting the angiotensin-converting enzyme (ACE), which plays a key role in the renin-angiotensin-aldosterone system (RAAS). Their mechanism of action includes:
- Reduction of angiotensin II formation, leading to vasodilation.
- Decreased secretion of aldosterone, resulting in reduced sodium and water retention.
- Lowering of blood pressure and reduced strain on the heart.
These effects make ACE inhibitors valuable in managing hypertension and heart failure.
These questions are tailored for experienced candidates in the field of Pharmacology, focusing on advanced topics and practical applications.
56. How do you approach the design of a clinical trial to ensure its scalability and efficiency?
When designing a clinical trial, scalability and efficiency can be ensured by focusing on several key aspects:
- Study Design: Choose an adaptive design that allows modifications based on interim results, which can enhance efficiency.
- Site Selection: Select multiple sites with experience in the therapeutic area to facilitate patient recruitment and data collection.
- Patient Stratification: Use biomarkers or genetic information to stratify patients, which can lead to more effective treatments and reduced variability.
- Data Management: Implement electronic data capture systems for real-time data access and monitoring, which streamlines operations and improves data integrity.
By prioritizing these elements, the clinical trial can remain flexible to changes while maximizing resource utilization and participant engagement.
57. What strategies do you recommend for mentoring junior pharmacologists in research methodologies?
Mentoring junior pharmacologists involves several effective strategies:
- Hands-On Training: Provide opportunities for direct involvement in research projects to enhance practical skills and understanding.
- Regular Feedback: Establish a routine for constructive feedback on their research progress, encouraging open communication about challenges faced.
- Resource Sharing: Introduce them to key literature, databases, and tools that are essential for pharmacological research.
- Goal Setting: Help them set achievable short-term and long-term research goals, fostering a sense of purpose and direction in their work.
These strategies not only build their competencies but also foster a collaborative environment that encourages continuous learning and professional growth.
How to Prepare for Your Pharmacology Interview
Preparing for a Pharmacology interview requires a strategic approach that encompasses understanding core concepts, staying updated on industry trends, and honing communication skills. This guide provides actionable tips to help you present your best self and demonstrate your expertise confidently.
- Familiarize yourself with key pharmacological concepts: Review essential topics such as drug classifications, mechanisms of action, pharmacokinetics, and pharmacodynamics. Having a solid grasp of these concepts will help you answer technical questions accurately and demonstrate your foundational knowledge.
- Stay updated on recent advancements: Research the latest developments in pharmacology, including new drug approvals, innovative therapies, and emerging research areas. This knowledge shows your commitment to the field and your ability to integrate current trends into your practice.
- Prepare for behavioral questions: Anticipate questions about teamwork, conflict resolution, and ethical dilemmas. Use the STAR method (Situation, Task, Action, Result) to structure your answers effectively, showcasing your problem-solving skills and ability to navigate real-world scenarios.
- Review case studies: Familiarize yourself with relevant case studies in pharmacology. Understand the clinical implications, patient management strategies, and drug interactions involved. This preparation will enhance your ability to discuss practical applications during the interview.
- Practice explaining complex concepts: Be ready to articulate complicated pharmacological principles in simple terms. Practicing these explanations will help you communicate effectively with both technical and non-technical audiences, showcasing your ability to educate others.
- Prepare questions for the interviewer: Develop thoughtful questions about the organization’s research focus, drug development pipeline, and team dynamics. Asking insightful questions demonstrates your genuine interest in the role and can help you assess if the position aligns with your career goals.
- Mock interviews: Conduct practice interviews with peers or mentors to simulate real interview conditions. Seek constructive feedback on your responses, body language, and overall presentation. This exercise can help boost your confidence and improve your performance on the actual interview day.
Common Pharmacology Interview Mistakes to Avoid
Preparing for a Pharmacology position can be challenging. Avoiding common interview mistakes is crucial to making a positive impression. Here’s a guide to help you navigate the interview process effectively and enhance your chances of success.
- Lack of Industry Knowledge: Failing to demonstrate an understanding of current trends and challenges in pharmacology can signal a lack of engagement. Research recent advancements and regulatory changes to showcase your knowledge and interest.
- Poor Communication Skills: Pharmacology often requires collaboration with diverse teams. Inability to clearly articulate your thoughts or explain complex concepts can hinder your effectiveness. Practice concise and clear communication to enhance your interview performance.
- Neglecting Behavioral Questions: Interviews often include behavioral questions assessing your problem-solving and teamwork skills. Prepare examples that highlight your experiences in overcoming challenges or working collaboratively in research or clinical settings.
- Not Asking Questions: Failing to ask insightful questions can indicate a lack of interest in the position or the company. Prepare thoughtful questions that reflect your interest in the role and the organization’s goals.
- Overlooking Soft Skills: Technical expertise is important, but soft skills like empathy, teamwork, and communication are equally crucial in pharmacology. Emphasize how your personal attributes contribute to effective collaboration and patient care.
- Inadequate Preparation for Technical Questions: Pharmacology interviews often include technical questions relevant to drug development and pharmacokinetics. Failing to review key concepts can lead to poor performance. Brush up on core pharmacological principles and recent research.
- Showing Lack of Enthusiasm: A lack of enthusiasm can negatively impact your candidacy. Demonstrate passion for pharmacology and a genuine interest in the role to create a more positive impression on the interviewer.
- Ignoring Follow-Up Etiquette: Not sending a thank-you note post-interview can be perceived as unprofessional. A timely follow-up expresses gratitude and reinforces your interest, helping you stand out from other candidates.
Key Takeaways for Pharmacology Interview Success
- Prepare your resume using an AI resume builder to ensure clarity and professionalism, highlighting your key pharmacology skills and experiences relevant to the position.
- Utilize resume templates to format your application materials consistently, making it easy for hiring managers to read and evaluate your qualifications quickly.
- Showcase your experience with effective resume examples that emphasize your accomplishments in pharmacology, demonstrating your ability to contribute value to the organization.
- Craft personalized cover letters that align your qualifications with the job requirements, illustrating your passion for pharmacology and your fit for the role.
- Engage in mock interview practice to refine your communication skills and prepare for common pharmacology-related questions, boosting your confidence during the actual interview.
Frequently Asked Questions
1. How long does a typical Pharmacology interview last?
A typical Pharmacology interview can last anywhere from 30 minutes to an hour. The duration often depends on the organization and the specific role. Interviews may include a mix of technical questions, behavioral assessments, and discussions about your research experience. It’s essential to be prepared for a variety of topics, as interviewers may delve into your background and knowledge in pharmacology, as well as your ability to think critically and solve problems in real-world scenarios.
2. What should I wear to a Pharmacology interview?
For a Pharmacology interview, it’s advisable to dress professionally to make a positive impression. Opt for business formal attire, such as a suit and tie for men or a tailored dress or suit for women. Choose neutral colors and avoid overly flashy accessories. Additionally, ensure that your clothing is clean and well-fitted. A polished appearance reflects your seriousness about the position and respect for the interviewers and the organization.
3. How many rounds of interviews are typical for a Pharmacology position?
Typically, a Pharmacology position may involve two to three rounds of interviews. The first round is often a screening interview, which may be conducted via phone or video call. Subsequent rounds may include in-person interviews with hiring managers and other team members, focusing on technical skills and cultural fit. Some organizations may also require a final interview with senior management. It’s crucial to prepare thoroughly for each stage to showcase your qualifications effectively.
4. Should I send a thank-you note after my Pharmacology interview?
Yes, it is important to send a thank-you note after your Pharmacology interview. This demonstrates your appreciation for the opportunity and reinforces your interest in the position. Aim to send your note within 24 hours of the interview. Keep it concise, expressing gratitude for the interviewer’s time, highlighting a key discussion point, and reiterating your enthusiasm for the role. A thoughtful thank-you note can leave a lasting positive impression and may set you apart from other candidates.