Preparing for a Pharmacovigilance interview requires a unique blend of scientific knowledge, regulatory understanding, and strong analytical skills. This role is vital in ensuring patient safety by monitoring and assessing drug safety throughout a product’s lifecycle. Given the critical nature of pharmacovigilance, thorough interview preparation is essential to articulate your expertise and demonstrate your commitment to patient well-being. This comprehensive guide will cover key topics such as essential knowledge areas, common interview questions, and strategies to showcase your skills effectively. By mastering these elements, you’ll enhance your confidence and significantly improve your chances of success in this rewarding field.
What to Expect in a Pharmacovigilance Interview
In a Pharmacovigilance interview, candidates can expect a mix of technical and behavioral questions to assess their knowledge of drug safety, regulatory requirements, and analytical skills. Interviews may be conducted by a panel of interviewers, including HR representatives, hiring managers, and experienced pharmacovigilance professionals. The structure typically begins with an introduction, followed by questions regarding the candidate’s background and specific pharmacovigilance scenarios. Candidates might also face situational questions to evaluate their problem-solving abilities. Some interviews may include case studies or role-playing exercises to simulate real-world challenges in drug safety monitoring.
Pharmacovigilance Interview Questions For Freshers
This set of interview questions is tailored for freshers pursuing a career in Pharmacovigilance. Candidates should focus on mastering fundamental concepts such as drug safety, adverse event reporting, regulatory compliance, and the tools used for data analysis in the field.
1. What is Pharmacovigilance?
Pharmacovigilance is the science and activities related to the detection, assessment, understanding, and prevention of adverse effects or any other drug-related problems. Its primary objective is to enhance patient safety and ensure that the benefits of a drug outweigh its risks throughout its lifecycle.
2. Why is adverse event reporting important?
Adverse event reporting is crucial as it helps in identifying, assessing, and minimizing risks associated with pharmaceuticals. This information aids regulatory authorities in making informed decisions regarding drug safety and efficacy, ultimately protecting public health by ensuring that unsafe drugs are withdrawn or better monitored.
3. What are the key components of a Pharmacovigilance system?
- Data Collection: Gathering information about adverse events from various sources.
- Data Analysis: Evaluating the collected data to identify patterns or signals of potential safety issues.
- Risk Management: Implementing strategies to mitigate identified risks.
- Reporting: Submitting findings to regulatory authorities as required.
These components work together to ensure ongoing drug safety monitoring and compliance with regulatory requirements.
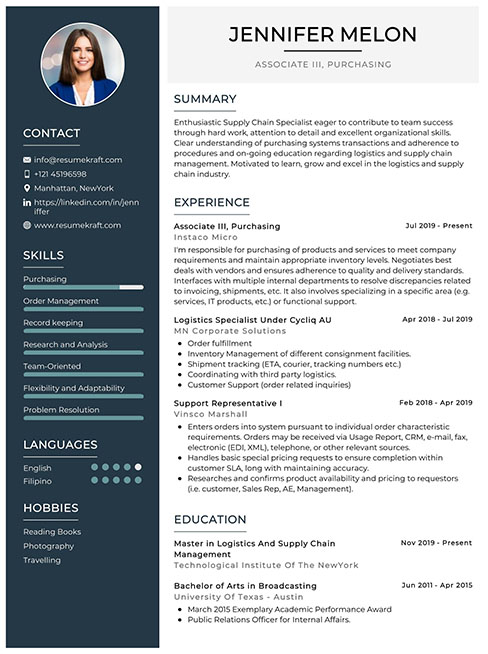
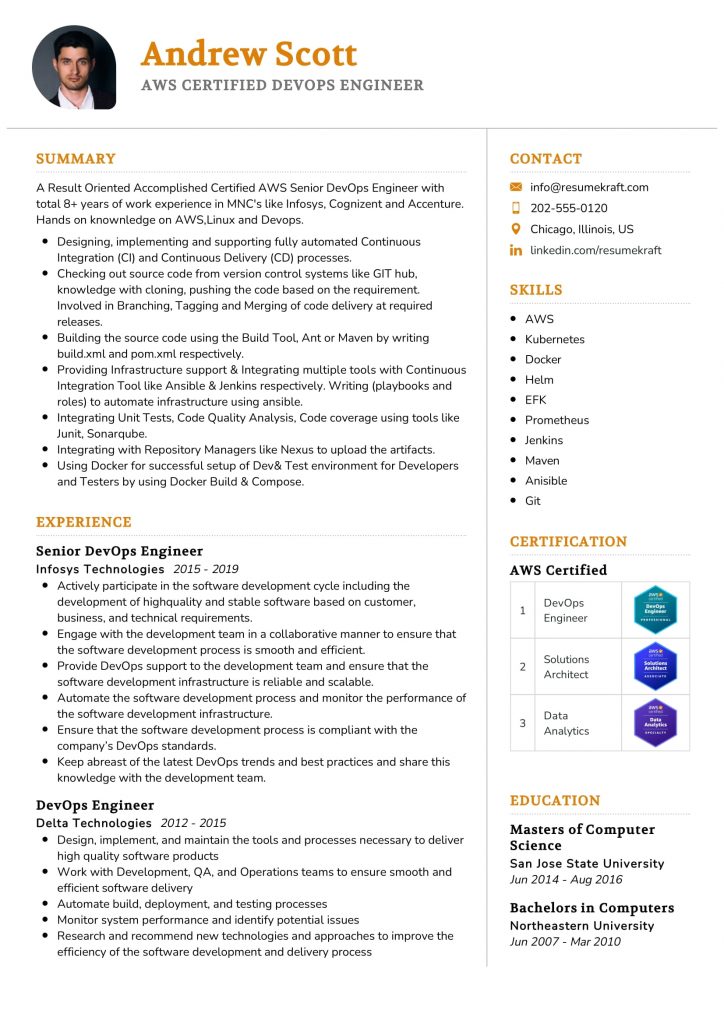
Build your resume in just 5 minutes with AI.
4. What is an adverse drug reaction (ADR)?
An adverse drug reaction (ADR) is an unwanted or harmful reaction experienced following the administration of a medication. ADRs can occur due to several factors, including the drug’s pharmacological properties, patient-specific variables, and drug interactions, and they can vary in severity from mild to life-threatening.
5. Explain the difference between a serious and a non-serious adverse event.
- Serious Adverse Event: Any adverse effect that results in death, is life-threatening, requires hospitalization, prolongs existing hospitalization, results in disability, or is a congenital anomaly.
- Non-Serious Adverse Event: Any adverse effect that does not meet the criteria for seriousness and typically resolves without significant medical intervention.
Understanding this distinction is essential for accurate reporting and risk assessment in pharmacovigilance.
6. What is a signal in pharmacovigilance?
A signal in pharmacovigilance refers to information that arises from one or multiple sources that suggests a new or known event may be associated with a drug, indicating a potential safety concern. Signal detection is a critical activity in pharmacovigilance, as it helps prioritize further investigation into drug safety.
7. Describe the role of regulatory authorities in pharmacovigilance.
Regulatory authorities, such as the FDA and EMA, play a vital role in pharmacovigilance by establishing guidelines for adverse event reporting, conducting safety evaluations, and monitoring drug safety. They also enforce compliance, review risk management plans, and require manufacturers to update product labeling based on new safety information.
8. What is the importance of the ICH E2E guidelines?
The ICH E2E guidelines provide a framework for the international harmonization of pharmacovigilance practices. They outline the responsibilities of pharmaceutical companies regarding safety data collection, reporting, and risk management, ensuring consistency and quality in pharmacovigilance activities across different regions.
9. What tools are commonly used in pharmacovigilance?
- Database Systems: Tools like Oracle Argus and VigiBase are used to manage and analyze adverse event data.
- Signal Detection Software: Software that helps identify potential signals in large datasets.
- Reporting Tools: Systems for creating and submitting reports to regulatory authorities.
These tools enhance the efficiency and accuracy of pharmacovigilance processes.
10. How do you assess the causality of an adverse event?
- Temporal Relationship: Determining if the adverse event occurred after the administration of the drug.
- Dechallenge/Rechallenge: Observing if symptoms resolve after discontinuation and recur upon re-administration.
- Other Factors: Considering known drug properties and patient history.
Causality assessment is crucial for understanding the relationship between a drug and an adverse event.
11. What is a Risk Management Plan (RMP)?
A Risk Management Plan (RMP) outlines the strategies to identify, characterize, prevent, or minimize risks associated with a drug. It includes information on risk assessment, risk minimization measures, and plans for post-marketing surveillance to ensure ongoing safety monitoring.
12. Explain the role of a Clinical Trial in pharmacovigilance.
Clinical trials are essential for pharmacovigilance as they provide the initial safety data on drugs before they are approved for public use. Ongoing monitoring during and after trials helps identify adverse events early, allowing for prompt action and adjustments to the drug’s risk management strategies.
13. What are some common challenges in pharmacovigilance?
- Data Quality: Ensuring the accuracy and completeness of reported data.
- Signal Detection: Identifying true safety signals amidst background noise.
- Regulatory Compliance: Adapting to changing regulations across different countries.
Addressing these challenges is key to effective pharmacovigilance and ensuring patient safety.
14. What ethical considerations are involved in pharmacovigilance?
Ethical considerations in pharmacovigilance include ensuring informed consent for participants in clinical trials, maintaining patient confidentiality, and the obligation to report adverse events promptly. Additionally, balancing the risks and benefits of drugs to protect public health is a fundamental ethical responsibility.
15. How can technology improve pharmacovigilance practices?
- Data Analytics: Advanced analytics can enhance signal detection and risk assessment.
- Artificial Intelligence: AI can automate data processing and improve the accuracy of reports.
- Real-time Monitoring: Technology enables continuous safety surveillance through real-time data collection.
Leveraging technology can significantly improve the efficiency and effectiveness of pharmacovigilance practices, ultimately enhancing drug safety.
These questions are designed for freshers entering the Pharmacovigilance field and cover fundamental concepts they should master.
16. What is Pharmacovigilance and why is it important?
Pharmacovigilance is the science and activities related to the detection, assessment, understanding, and prevention of adverse effects or any other drug-related problems. It is crucial for ensuring drug safety, assessing risk, and promoting safe medication use. Effective pharmacovigilance helps protect patients by monitoring drug safety after market approval and contributes to public health by informing regulatory actions and clinical practices.
17. What are some common adverse drug reactions (ADRs)?
- Allergic Reactions: These can range from mild rashes to severe anaphylaxis, depending on the individual’s sensitivity to a drug.
- Gastrointestinal Issues: Common ADRs include nausea, vomiting, diarrhea, and constipation, which can occur due to various medications.
- CNS Effects: Some drugs may cause sedation, dizziness, or confusion, particularly in the elderly or those with underlying conditions.
- Cardiovascular Reactions: Certain medications may lead to changes in blood pressure, heart rate irregularities, or other cardiovascular issues.
Recognizing these ADRs is essential for healthcare professionals to manage patient safety effectively and make informed decisions about medication use.
18. What are the key components of a Pharmacovigilance system?
- Data Collection: Gathering information about adverse events from various sources including healthcare providers, patients, and clinical trials.
- Data Assessment: Evaluating the collected data to determine the causal relationship between the drug and the adverse event.
- Risk Management: Developing strategies to minimize risks associated with drug use, including labeling changes and risk communication.
- Regulatory Reporting: Submitting reports to regulatory authorities in compliance with local and international guidelines.
These components work together to ensure the continuous monitoring of drug safety and the well-being of patients.
19. How do you report an adverse event in Pharmacovigilance?
To report an adverse event in Pharmacovigilance, one typically follows these steps:
- Gather Information: Collect detailed information about the patient, the medication involved, the adverse event, and any other relevant clinical data.
- Use Reporting Tools: Fill out a standardized adverse event reporting form, which may vary by country or organization.
- Submit the Report: Send the completed report to the appropriate pharmacovigilance authority or the pharmaceutical company responsible for the drug.
Timely reporting is essential to ensure effective monitoring and management of drug safety.
20. What role do regulatory authorities play in Pharmacovigilance?
Regulatory authorities, such as the FDA in the United States or EMA in Europe, play a critical role in Pharmacovigilance by:
- Setting Guidelines: They establish regulations and guidelines for drug safety monitoring and reporting adverse events.
- Reviewing Data: Authorities assess safety data submitted by pharmaceutical companies to evaluate risk-benefit profiles of medications.
- Taking Action: They can impose restrictions, issue safety alerts, or even withdraw drugs from the market if necessary to protect public health.
Their oversight is vital for maintaining drug safety and ensuring public trust in the healthcare system.
21. What is the difference between a serious and non-serious adverse event?
A serious adverse event (SAE) is one that results in significant outcomes such as death, hospitalization, life-threatening situations, or permanent disability. Non-serious adverse events are less severe and do not have lasting health impacts, such as mild nausea or a temporary rash. Understanding this distinction is essential for prioritizing safety assessments and regulatory reporting in Pharmacovigilance.
Pharmacovigilance Intermediate Interview Questions
This section covers intermediate-level Pharmacovigilance interview questions, focusing on essential concepts and practical applications candidates should be familiar with. Understanding drug safety regulations, adverse event reporting, and risk management principles is crucial for success in this field.
22. What is Pharmacovigilance and why is it important?
Pharmacovigilance is the science and activities related to the detection, assessment, understanding, and prevention of adverse effects or any other drug-related problems. Its importance lies in ensuring patient safety and improving the safe use of medicines. This includes monitoring drug safety post-marketing, identifying potential risks, and taking necessary actions to mitigate harm to patients.
23. Can you explain the difference between adverse event and adverse drug reaction?
An adverse event (AE) refers to any undesirable experience associated with the use of a medical product in a patient, regardless of whether it is related to the product. In contrast, an adverse drug reaction (ADR) is a harmful or unintended response to a drug that occurs at normal doses. Understanding this distinction is crucial for accurate reporting and assessment.
24. What are the key components of a pharmacovigilance system?
- Data Collection: Gathering information on adverse events from various sources.
- Data Management: Organizing and analyzing the collected data for trends and patterns.
- Risk Assessment: Evaluating the safety profile of drugs based on reported events.
- Signal Detection: Identifying potential safety issues that may require further investigation.
- Regulatory Reporting: Submitting findings to regulatory authorities as required.
These components work together to ensure a comprehensive approach to monitoring drug safety.
25. How do you conduct a signal detection in pharmacovigilance?
Signal detection involves analyzing data from adverse event reports to identify potential safety issues. This can be done using statistical methods and data mining techniques. Common approaches include disproportionality analysis, Bayesian data mining, and the use of software tools to visualize data trends. The goal is to determine whether there is enough evidence to warrant further investigation into a specific safety concern.
26. Describe the role of the Risk Management Plan (RMP) in pharmacovigilance.
The Risk Management Plan (RMP) is a regulatory document that outlines the risk assessment and minimization strategies for a drug. It includes information on known risks, risk mitigation measures, and plans for monitoring the effectiveness of these measures. The RMP is crucial for ensuring that all potential risks associated with a drug are managed appropriately throughout its lifecycle.
27. What are the ICH E2E guidelines?
The ICH E2E guidelines provide a framework for pharmacovigilance practices, ensuring consistent safety reporting and risk management across different regions. They emphasize the importance of a proactive approach to monitoring adverse events, the need for a well-structured pharmacovigilance system, and the integration of safety data into the overall drug development process.
28. Explain the concept of benefit-risk assessment.
Benefit-risk assessment is a systematic evaluation of the positive effects of a drug against its potential risks. This assessment helps regulatory authorities and healthcare professionals make informed decisions about whether to approve, continue, or withdraw a drug from the market. Factors considered include the severity and frequency of adverse events and the therapeutic benefits provided by the drug.
29. What role does MedDRA play in pharmacovigilance?
MedDRA (Medical Dictionary for Regulatory Activities) is a standardized medical terminology used in pharmacovigilance to classify and code adverse events. It facilitates the consistent reporting and analysis of safety data across different stakeholders, enabling better communication and understanding of drug safety issues. MedDRA helps ensure that adverse events are accurately categorized and reported.
30. How do you ensure compliance with regulatory requirements in pharmacovigilance?
- Stay Updated: Regularly review and understand relevant regulatory guidelines and updates.
- Training: Provide ongoing training for staff on compliance procedures and regulatory expectations.
- Audits: Conduct internal audits to ensure adherence to pharmacovigilance protocols.
- Documentation: Maintain thorough and accurate records of all pharmacovigilance activities.
These practices help maintain compliance and enhance the integrity of the pharmacovigilance system.
31. What is a Clinical Trial Safety Report (CTSR)?
A Clinical Trial Safety Report (CTSR) is a document that summarizes safety information for investigational medicinal products during clinical trials. It includes details on adverse events, serious adverse events, and any risk management activities undertaken. CTSRs are essential for monitoring the safety of trial participants and ensuring compliance with regulatory reporting requirements.
32. Describe the significance of the World Health Organization’s (WHO) pharmacovigilance program.
The WHO pharmacovigilance program aims to improve patient safety and ensure the safe use of medicines globally. It provides a framework for countries to report adverse drug reactions and share safety information. This program fosters collaboration among countries, promotes the use of standardized reporting systems, and enhances the quality of safety data collected worldwide.
33. What is the role of the Data Safety Monitoring Board (DSMB)?
The Data Safety Monitoring Board (DSMB) is an independent group that monitors patient safety and treatment efficacy during a clinical trial. The DSMB reviews interim data and can recommend modifications to the trial, including stopping it if safety concerns arise. Their oversight is critical for protecting participants and ensuring ethical conduct throughout the study.
34. Explain the term “dechallenge” and “rechallenge” in pharmacovigilance.
- Dechallenge: This refers to the process of withdrawing a drug from a patient after an adverse event occurs to determine if the event resolves upon discontinuation.
- Rechallenge: This involves re-administering the drug to the patient after the adverse event has resolved to see if the event recurs, providing further evidence of causality.
Both processes are essential for establishing a causal relationship between a drug and an adverse event.
35. What are periodic safety update reports (PSURs)?
Periodic Safety Update Reports (PSURs) are documents that provide an update on the safety profile of a drug following its approval. They summarize the findings from pharmacovigilance activities, including new safety data, significant risks, and benefit-risk assessments. PSURs are submitted to regulatory authorities at defined intervals to ensure ongoing monitoring of drug safety.
Here are six intermediate-level interview questions focused on Pharmacovigilance, designed to test knowledge of practical applications and real-world scenarios.
37. What is the role of a Data Management System in Pharmacovigilance?
A Data Management System (DMS) in Pharmacovigilance plays a crucial role in the collection, management, and analysis of adverse event data. It ensures that data is stored securely and can be accessed efficiently for reporting and regulatory compliance. The system facilitates data validation, integration from various sources, and supports data mining techniques to identify potential safety signals, thus aiding in risk assessment and decision-making processes.
38. Can you explain what signal detection is in Pharmacovigilance?
Signal detection in Pharmacovigilance refers to the process of identifying and evaluating potential safety concerns related to pharmaceutical products. This involves analyzing data from various sources, such as spontaneous reports, clinical trials, and literature. The key steps include:
- Data Collection: Gathering adverse event reports from healthcare providers and patients.
- Data Analysis: Employing statistical methods to identify patterns or anomalies that may indicate a safety issue.
- Signal Validation: Assessing the clinical significance of detected signals and determining whether further investigation is warranted.
The goal is to ensure patient safety and make informed decisions regarding product labeling and risk management.
39. What are the main regulatory requirements for reporting adverse events in Pharmacovigilance?
The main regulatory requirements for reporting adverse events vary by region but generally include the following key components:
- Timeliness: Adverse events must be reported within specific timelines (e.g., 7 days for serious events in the EU).
- Content: Reports should contain detailed information, including patient demographics, event descriptions, and product details.
- Follow-up: Companies are required to conduct follow-up investigations on reported events to gather additional information.
- Compliance: Adherence to local regulations (such as FDA in the U.S. and EMA in Europe) is mandatory for maintaining market authorization.
These requirements ensure consistent monitoring and reporting of product safety to protect public health.
40. Describe the importance of a Risk Management Plan (RMP) in Pharmacovigilance.
A Risk Management Plan (RMP) is critical in Pharmacovigilance as it outlines the strategies to identify, characterise, prevent, or minimize risks associated with a drug. Key aspects include:
- Risk Identification: Recognizing potential risks based on clinical data and post-marketing experience.
- Risk Minimization: Implementing measures such as additional warnings, educational programs for healthcare professionals, or restricted distribution.
- Monitoring Effectiveness: Establishing mechanisms to assess the effectiveness of risk minimization strategies over time.
RMPs are essential for ensuring ongoing safety and efficacy of pharmaceutical products throughout their lifecycle.
41. What is the role of database queries in Pharmacovigilance data analysis?
Database queries are pivotal in Pharmacovigilance data analysis as they help extract relevant information from large datasets. Common roles include:
- Data Retrieval: Queries can be used to isolate specific adverse event reports based on criteria such as drug name, event type, or demographic data.
- Signal Detection: By querying databases, analysts can identify trends and correlations that signal potential safety issues.
- Reporting: Queries facilitate the generation of compliance reports and submissions to regulatory authorities.
Effective querying techniques enhance the quality of pharmacovigilance analyses and support timely safety assessments.
Build your resume in 5 minutes
Our resume builder is easy to use and will help you create a resume that is ATS-friendly and will stand out from the crowd.
42. How do you ensure data quality in Pharmacovigilance reporting?
Ensuring data quality in Pharmacovigilance reporting involves implementing several best practices:
- Standardization: Use standardized data collection forms and coding systems (like MedDRA) to minimize variability.
- Training: Regularly train staff on data entry protocols and the importance of accurate reporting.
- Regular Audits: Conduct periodic audits and reviews of reported data to identify and correct discrepancies.
- Automated Checks: Employ automated validation checks within data management systems to flag potential errors during entry.
These measures help maintain high data integrity, which is vital for accurate safety monitoring and regulatory compliance.
Pharmacovigilance Interview Questions for Experienced
This set of Pharmacovigilance interview questions is tailored for experienced professionals, focusing on advanced topics such as risk management strategies, regulatory compliance, signal detection methodologies, and leadership in the Pharmacovigilance field. Candidates should be prepared to discuss complex scenarios and demonstrate their expertise in these areas.
43. What are the key components of a Pharmacovigilance system?
A comprehensive Pharmacovigilance system includes several key components:
- Data Collection: Gathering adverse event reports from various sources such as clinical trials, post-marketing surveillance, and literature reviews.
- Data Processing: Assessing and categorizing the data to identify potential safety issues or signals.
- Risk Assessment: Evaluating the significance of the identified signals to determine if regulatory action is necessary.
- Regulatory Reporting: Reporting findings to regulatory authorities as per legal requirements.
- Risk Communication: Informing stakeholders, including healthcare professionals and patients, about risks associated with products.
This system ensures patient safety and compliance with regulatory standards.
44. How do you approach signal detection in Pharmacovigilance?
Signal detection involves identifying safety signals from aggregated data. The approach includes:
- Statistical Methods: Utilizing statistical tools like Bayesian data mining and disproportionality analysis to detect signals.
- Clinical Judgment: Applying clinical expertise to contextualize the data and validate signals.
- Data Sources: Employing multiple data sources such as spontaneous reports, electronic health records, and literature.
An effective signal detection strategy is crucial for timely interventions to ensure patient safety.
45. Can you explain the importance of risk management plans (RMPs) in Pharmacovigilance?
Risk Management Plans (RMPs) are essential as they outline the risk assessment and minimization strategies for medicinal products. Key aspects include:
- Identifying Risks: Detailing potential risks associated with a product.
- Mitigation Strategies: Outlining strategies to mitigate identified risks, including additional monitoring or risk communication.
- Evaluation: Describing how the effectiveness of risk minimization measures will be assessed over time.
RMPs ensure that safety considerations are integrated into the product lifecycle and regulatory compliance.
46. What are the challenges of data integration in Pharmacovigilance?
Data integration in Pharmacovigilance faces several challenges, including:
- Data Quality: Ensuring accuracy, completeness, and consistency of data from diverse sources.
- Standardization: Achieving uniformity in data formats and terminologies across platforms.
- Regulatory Compliance: Navigating differing regulatory requirements for data sharing and integration.
- Technical Complexity: Handling the technical challenges associated with large datasets, including data storage and processing capabilities.
Addressing these challenges is vital for effective signal detection and patient safety.
47. Describe how you would mentor a junior Pharmacovigilance professional.
Mentoring a junior professional involves several key strategies:
- Knowledge Sharing: Providing insights into best practices, regulatory requirements, and industry trends.
- Practical Experience: Involving them in real-world projects to apply their knowledge and develop skills.
- Feedback Mechanism: Offering constructive feedback on their work to foster improvement.
- Career Guidance: Assisting them in setting career goals and providing resources for professional development.
Effective mentoring contributes to building a competent and confident Pharmacovigilance workforce.
48. What design patterns are commonly used in Pharmacovigilance software development?
In Pharmacovigilance software development, several design patterns are commonly employed:
- Model-View-Controller (MVC): Separates application logic from user interface, enhancing maintainability.
- Observer Pattern: Allows for efficient notification of changes in data across the application.
- Singleton Pattern: Ensures a single instance of a class is used for managing shared resources, such as database connections.
These patterns promote scalability and maintainability in Pharmacovigilance systems, which handle large volumes of data.
49. How do you ensure compliance with regulatory requirements in Pharmacovigilance?
Ensuring compliance involves several key steps:
- Understanding Regulations: Keeping up-to-date with local and international regulations such as ICH E2E and FDA guidelines.
- Training: Providing regular training for the team on compliance standards and practices.
- Audit Processes: Implementing internal audits to identify gaps in compliance and address them proactively.
- Documentation: Maintaining comprehensive and accurate records of all Pharmacovigilance activities.
Compliance is critical for the integrity of Pharmacovigilance systems and the safety of patients.
50. Discuss the role of technology in enhancing Pharmacovigilance processes.
Technology plays a crucial role in enhancing Pharmacovigilance processes by:
- Data Analytics: Leveraging big data analytics to identify safety signals more effectively.
- Automation: Automating data collection and reporting processes to improve efficiency and reduce errors.
- Artificial Intelligence: Utilizing AI and machine learning to predict adverse events based on historical data.
These technological advancements lead to more efficient and effective Pharmacovigilance operations, improving patient safety outcomes.
51. How do you handle discrepancies in adverse event reports?
Handling discrepancies involves a systematic approach:
- Investigation: Conducting a thorough investigation to identify the source of the discrepancy.
- Cross-Verification: Checking data against multiple sources to validate findings.
- Documentation: Documenting all findings and decisions made during the investigation.
- Communication: Informing relevant stakeholders about discrepancies and actions taken.
This approach ensures transparency and maintains the integrity of the Pharmacovigilance process.
52. What strategies would you implement to improve the quality of safety data?
Improving the quality of safety data can be achieved through several strategies:
- Training Programs: Conducting regular training for staff on data entry and reporting standards.
- Standard Operating Procedures (SOPs): Developing clear SOPs for data collection and management.
- Quality Control Checks: Implementing routine audits and quality checks to identify and rectify errors.
- Feedback Loops: Creating a feedback mechanism for continuous improvement based on collected data.
These strategies enhance the reliability and accuracy of safety data in Pharmacovigilance.
53. Describe the process of preparing a safety report for regulatory submission.
The process for preparing a safety report includes several critical steps:
- Data Compilation: Gathering all relevant data from various sources, including adverse event reports and clinical studies.
- Signal Assessment: Evaluating the data to identify any new or evolving safety signals.
- Report Writing: Drafting the report in accordance with regulatory requirements and guidelines.
- Internal Review: Conducting an internal review to ensure accuracy and completeness before submission.
- Submission: Submitting the report to the appropriate regulatory authority within specified timelines.
This thorough process ensures compliance and enhances patient safety monitoring.
54. How do you approach stakeholder engagement in Pharmacovigilance?
Engaging stakeholders involves several key strategies:
- Regular Communication: Maintaining open lines of communication with healthcare professionals, regulatory bodies, and patients.
- Feedback Collection: Actively seeking feedback from stakeholders to understand their concerns and expectations.
- Educational Initiatives: Providing educational resources and updates on safety information to stakeholders.
- Collaboration: Collaborating with stakeholders for joint initiatives aimed at improving drug safety.
Effective stakeholder engagement fosters trust and enhances the overall effectiveness of Pharmacovigilance efforts.
55. What are the emerging trends in Pharmacovigilance that professionals should be aware of?
Emerging trends in Pharmacovigilance include:
- Real-World Evidence: Increasing reliance on real-world data to inform safety assessments and decision-making.
- Digital Health Technologies: Integration of digital tools such as mobile applications for direct patient reporting of adverse events.
- Artificial Intelligence: Use of AI in signal detection and risk assessment to enhance accuracy and efficiency.
- Patient-Centric Approaches: Focusing on patient involvement in safety reporting and risk management.
Staying informed about these trends is crucial for professionals to adapt to the evolving landscape of Pharmacovigilance.
Below is a critical interview question designed for experienced professionals in the field of Pharmacovigilance. This question focuses on important aspects of the role, including leadership and optimization strategies.
58. How do you ensure the effective management and reporting of adverse drug reactions (ADRs) in a pharmacovigilance system?
Effective management and reporting of ADRs in a pharmacovigilance system can be ensured through several key strategies:
- Standard Operating Procedures (SOPs): Establish clear and comprehensive SOPs for collecting, assessing, and reporting ADRs to ensure consistency and compliance with regulatory requirements.
- Training and Development: Regular training sessions for staff on the latest regulations and best practices in pharmacovigilance to enhance their skills and knowledge.
- Data Management Systems: Implement robust data management systems that allow for efficient data entry, retrieval, and analysis of ADR reports, facilitating timely reporting.
- Collaboration with Stakeholders: Foster strong communication with healthcare professionals, patients, and regulatory bodies to ensure all ADRs are reported and investigated thoroughly.
- Continuous Monitoring: Utilize advanced analytics and machine learning techniques to monitor data trends and identify potential safety signals swiftly.
By integrating these strategies, a pharmacovigilance system can enhance its efficiency and effectiveness, ultimately leading to improved patient safety and regulatory compliance.
How to Prepare for Your Pharmacovigilance Interview
Preparing for a Pharmacovigilance interview requires a thorough understanding of drug safety, regulatory guidelines, and industry practices. Focus on relevant experiences, knowledge of safety databases, and the ability to analyze data, as these are critical for success in this field.
- Familiarize yourself with key pharmacovigilance regulations such as ICH-GCP, FDA, and EMA guidelines. Understanding these frameworks is crucial as they govern the reporting and management of adverse drug reactions and ensure compliance with safety standards.
- Review the latest trends and developments in drug safety. Being knowledgeable about current events, new technologies, and advancements in pharmacovigilance demonstrates your commitment to the field and can set you apart from other candidates.
- Prepare to discuss your experience with safety databases and software tools, such as Argus or Oracle. Highlight specific instances where you utilized these tools to manage data or report adverse events, showcasing your technical proficiency.
- Practice behavioral interview questions that explore your problem-solving skills and ability to work under pressure. Situations like handling a safety signal or managing multiple cases can help illustrate your critical thinking and decision-making abilities.
- Be ready to explain complex scientific concepts related to drug safety in simple terms. Interviewers often assess your ability to communicate effectively with both technical and non-technical stakeholders, making this skill vital for a successful Pharmacovigilance specialist.
- Network with professionals in the field. Engaging in discussions about best practices and challenges can provide valuable insights and may lead to important connections, which can be beneficial during your job search and interview process.
- Prepare thoughtful questions to ask your interviewers about their pharmacovigilance processes and team dynamics. This shows your genuine interest in the role and helps you assess if the company’s culture aligns with your career goals.
Common Pharmacovigilance Interview Mistakes to Avoid
When interviewing for a Pharmacovigilance position, candidates often make critical mistakes that can hinder their chances of success. Understanding these common pitfalls can help applicants present themselves more effectively and demonstrate their qualifications in this specialized field.
- Not Understanding Regulatory Guidelines: Failing to familiarize yourself with key regulations such as FDA, EMA, or ICH guidelines can indicate a lack of commitment to the field. Knowledge of these regulations is crucial for ensuring drug safety.
- Neglecting Industry Terminology: Using incorrect or outdated terminology related to Pharmacovigilance may suggest a lack of current knowledge. Familiarity with terms like adverse events, signal detection, and risk management is essential for effective communication.
- Overlooking Soft Skills: Focusing solely on technical expertise while neglecting soft skills like communication and teamwork can be a mistake. Pharmacovigilance often requires collaboration with various stakeholders, making interpersonal skills vital.
- Insufficient Preparation for Behavioral Questions: Not preparing for behavioral questions can lead to vague or unsatisfactory responses. Interviewers seek specific examples of past experiences to assess your problem-solving and decision-making abilities.
- Failure to Discuss Relevant Experience: Not highlighting your specific experience in Pharmacovigilance or related fields can weaken your candidacy. Clearly articulating relevant projects or roles demonstrates your suitability for the position.
- Ignoring the Importance of Data Analysis: Underestimating the role of data analysis can be detrimental. Candidates should showcase their analytical skills and familiarity with data management tools used in Pharmacovigilance.
- Not Asking Insightful Questions: Failing to ask thoughtful questions about the role or the company can indicate a lack of genuine interest. Engaging with the interviewer through insightful questions shows your enthusiasm and understanding of the field.
- Being Unprepared for Case Studies: Many interviews include case studies to assess analytical thinking. Being unprepared for these scenarios can lead to weak performance, so practicing case study questions is essential.
Key Takeaways for Pharmacovigilance Interview Success
- Thoroughly prepare your resume using an AI resume builder to highlight your key skills and experiences in Pharmacovigilance, ensuring it meets industry standards for clarity and relevance.
- Choose appropriate resume templates that reflect your professionalism and the specific requirements of the Pharmacovigilance role you are applying for, making your application visually appealing.
- Showcase your experience with specific resume examples that demonstrate your knowledge of drug safety practices and regulatory compliance, enhancing your credibility during the interview.
- Craft tailored cover letters that align with the job description, emphasizing your passion for Pharmacovigilance and detailing how your background makes you a strong fit for the position.
- Engage in mock interview practice to build confidence and refine your responses to common Pharmacovigilance questions, helping you articulate your expertise effectively during the actual interview.
Frequently Asked Questions
1. How long does a typical Pharmacovigilance interview last?
A typical Pharmacovigilance interview lasts between 30 to 60 minutes. The duration can vary depending on the organization and the role level. Interviews may include a mix of behavioral questions, technical expertise discussions, and situational questions related to drug safety. It’s important to prepare for both general questions about your background and specific questions that assess your knowledge of pharmacovigilance processes, regulations, and case handling.
2. What should I wear to a Pharmacovigilance interview?
For a Pharmacovigilance interview, it is advisable to dress in professional business attire. This typically means wearing a tailored suit, dress shirt, and polished shoes for men, while women can opt for a suit or a professional dress. Dressing professionally shows your seriousness about the position and demonstrates respect for the interview process. Always ensure your outfit is clean, well-fitted, and appropriate for the company’s culture, which you can gauge from their website or social media.
3. How many rounds of interviews are typical for a Pharmacovigilance position?
Typically, a Pharmacovigilance position may involve two to three rounds of interviews. The first round is often a screening interview conducted by HR to assess your fit for the role and organization. Subsequent rounds usually involve technical interviews with hiring managers or team leads who evaluate your expertise in pharmacovigilance practices, regulations, and relevant case studies. Some companies may also include a final round focused on cultural fit within the team.
4. Should I send a thank-you note after my Pharmacovigilance interview?
Yes, sending a thank-you note after your Pharmacovigilance interview is highly recommended. It expresses gratitude for the opportunity and reinforces your interest in the position. A concise note can highlight key points from the interview and reiterate your enthusiasm for the role. Aim to send your thank-you note within 24 hours of the interview, whether via email or a handwritten note, as this can leave a positive impression on the interviewers.