Preparing for a Physical Therapist interview is a crucial step towards launching a rewarding career in healthcare. This role is unique as it blends scientific knowledge with compassionate patient care, requiring not only expertise in anatomy and rehabilitation techniques but also the ability to communicate effectively and inspire confidence in patients. Proper interview preparation can make a significant difference, helping candidates articulate their skills, experiences, and understanding of patient needs. This comprehensive guide will cover common interview questions, effective strategies for answering them, and tips for showcasing your qualifications and passion for helping others in the physical therapy field.
- What to Expect in a Physical Therapist Interview
- Physical Therapist Interview Questions For Freshers
- Physical Therapist Intermediate Interview Questions
- Physical Therapist Interview Questions for Experienced
- How to Prepare for Your Physical Therapist Interview
- Common Physical Therapist Interview Mistakes to Avoid
- Key Takeaways for Physical Therapist Interview Success
- Frequently Asked Questions
What to Expect in a Physical Therapist Interview
In a Physical Therapist interview, candidates can expect a mix of behavioral and clinical questions, often conducted by a panel of interviewers including hiring managers, senior therapists, and sometimes human resources personnel. The interview typically starts with an overview of the candidate’s background followed by scenario-based questions to assess problem-solving skills and clinical reasoning. Candidates may also be asked about their treatment philosophies and experience with specific patient populations. Additionally, practical assessments or role-playing scenarios may be included to evaluate hands-on skills and patient interaction techniques.
Physical Therapist Interview Questions For Freshers
Preparing for a physical therapist interview involves understanding key concepts and practices in the field. Freshers should master foundational knowledge related to patient assessment, treatment techniques, rehabilitation protocols, and ethical standards to excel in their interviews and future careers.
1. What is the role of a physical therapist?
A physical therapist (PT) is a healthcare professional who helps patients improve their movement and manage pain through various therapeutic methods. They assess patients’ physical conditions, develop treatment plans, and provide rehabilitation services to restore mobility and function after injuries or surgeries. PTs also educate patients on injury prevention and overall wellness.
2. Explain the importance of patient assessment in physical therapy.
Patient assessment is crucial in physical therapy as it helps therapists understand the patient’s condition, identify impairments, and set appropriate treatment goals. This process typically includes taking a detailed medical history, performing physical examinations, and utilizing various assessment tools to evaluate strength, flexibility, and range of motion.
3. What are common treatment modalities used in physical therapy?
- Exercise Therapy: Involves specific exercises to improve strength, flexibility, and balance.
- Manual Therapy: Hands-on techniques to relieve pain and improve mobility.
- Electrotherapy: Uses electrical energy for pain relief and muscle stimulation.
- Ultrasound Therapy: Employs sound waves to promote tissue healing.
These modalities can be used in combination to create a comprehensive treatment plan tailored to each patient’s needs.
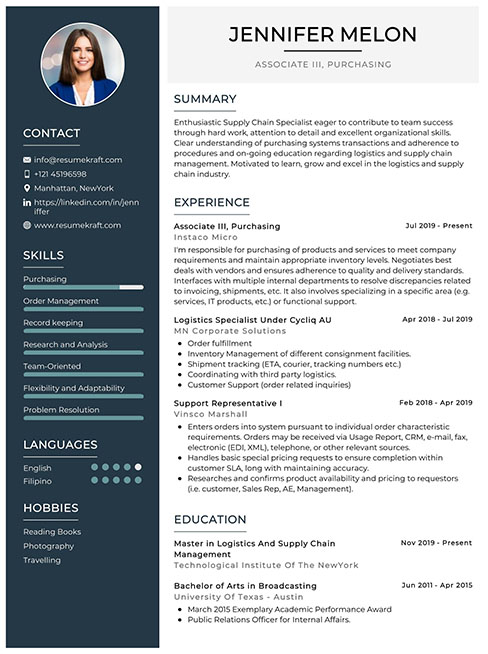
Build your resume in just 5 minutes with AI.
4. How do you approach a treatment plan for a new patient?
When creating a treatment plan for a new patient, I first conduct a thorough assessment to understand their specific condition and needs. After gathering relevant information, I collaborate with the patient to establish achievable goals. I then outline a personalized treatment schedule that includes exercises, interventions, and education, ensuring the plan is adaptable based on the patient’s progress.
5. What are some common conditions treated by physical therapists?
- Musculoskeletal injuries: Sprains, strains, and fractures.
- Neurological disorders: Stroke, multiple sclerosis, and Parkinson’s disease.
- Post-surgical rehabilitation: Recovery following orthopedic surgeries.
- Chronic pain conditions: Arthritis and back pain.
Physical therapists play a vital role in managing these conditions to improve patients’ quality of life.
6. How do you educate patients on exercise and rehabilitation?
Educating patients on exercise and rehabilitation involves explaining the purpose and benefits of each exercise, demonstrating proper techniques, and providing written instructions. I encourage questions to ensure understanding and highlight the importance of adherence to their rehabilitation program. Additionally, I discuss how lifestyle changes can enhance their recovery and overall well-being.
7. What is the significance of documentation in physical therapy?
Documentation is essential in physical therapy for several reasons: it provides a legal record of patient care, tracks progress over time, and ensures continuity of care among providers. Accurate documentation helps in assessing the effectiveness of treatment plans and is often required for insurance reimbursement. It also aids in communicating with other healthcare professionals.
8. Describe the ethical guidelines that physical therapists must follow.
- Patient Privacy: Respecting confidentiality and safeguarding patient information.
- Informed Consent: Ensuring patients understand their treatment options and giving consent.
- Professional Integrity: Providing care based on evidence and avoiding conflicts of interest.
- Competence: Continuing education to maintain and enhance professional skills.
Adhering to these guidelines is crucial for building trust and ensuring high-quality care.
9. How do you handle difficult patients?
Handling difficult patients requires patience, empathy, and effective communication. I try to understand their concerns and frustrations, actively listen to their feedback, and validate their feelings. Establishing a rapport and maintaining a positive attitude can help de-escalate situations. Additionally, I focus on clear communication about treatment goals and expectations to foster cooperation.
10. What role does teamwork play in physical therapy?
Teamwork is vital in physical therapy as PTs often collaborate with other healthcare professionals, such as physicians, occupational therapists, and nurses. Effective communication and collaboration enhance patient care, ensure comprehensive treatment plans, and facilitate better outcomes. By working together, we can share insights and leverage each other’s expertise to optimize patient recovery.
11. What are the key components of a rehabilitation program?
- Goal Setting: Establishing clear, measurable objectives for recovery.
- Exercise Prescription: Tailoring exercises to improve strength and function.
- Progress Monitoring: Regularly assessing the patient’s improvement and adjusting the program as needed.
- Patient Education: Instructing patients on self-management strategies and home exercises.
A well-rounded rehabilitation program addresses the patient’s unique needs and promotes optimal recovery.
12. How do you stay updated with the latest research and advancements in physical therapy?
To stay updated, I regularly read professional journals, attend workshops and conferences, and participate in continuing education courses. Networking with peers and engaging in online forums also helps me stay informed about new practices and evidence-based approaches in physical therapy. This commitment to lifelong learning is essential for providing the best care to my patients.
13. Can you explain the concept of evidence-based practice in physical therapy?
Evidence-based practice (EBP) in physical therapy involves integrating the best available research evidence with clinical expertise and patient preferences to inform treatment decisions. This approach ensures that interventions are grounded in scientific research, which enhances patient outcomes and promotes effective and efficient care. EBP encourages PTs to critically evaluate and apply research findings to their practice.
14. What are the common challenges faced by physical therapists?
- Patient Compliance: Ensuring patients adhere to their prescribed treatment plans can be challenging.
- Workplace Stress: Managing a high caseload and administrative tasks can lead to burnout.
- Keeping Up with Research: Staying current with advancements in physical therapy requires ongoing effort.
Addressing these challenges is essential for maintaining quality care and personal well-being in the profession.
15. How do you approach continuing education in your career?
Continuing education is a priority in my career, as it enhances my skills and knowledge in physical therapy. I actively seek out opportunities for professional development, including attending workshops, obtaining certifications, and participating in online courses. Engaging in lifelong learning not only improves my practice but also benefits my patients through the application of current best practices.
These questions are designed for freshers entering the Physical Therapy field and cover fundamental concepts they should master.
16. What is the primary goal of physical therapy?
The primary goal of physical therapy is to help patients improve their physical function and quality of life. This includes reducing pain, restoring mobility, enhancing strength, and preventing future injuries. Physical therapists assess each patient’s needs and develop personalized treatment plans that may include exercises, manual therapy, education, and modalities such as heat or ice therapy.
17. What are some common techniques used in physical therapy?
- Therapeutic Exercises: Customized exercises designed to improve strength, flexibility, and endurance.
- Manual Therapy: Hands-on techniques used to manipulate muscles and joints to relieve pain and improve mobility.
- Modalities: Use of heat, ice, ultrasound, and electrical stimulation to reduce pain and promote healing.
- Education: Teaching patients about their conditions and self-management strategies.
These techniques are often combined to create a comprehensive treatment plan tailored to the individual’s specific needs.
18. How do you assess a patient’s condition before treatment?
Assessing a patient’s condition involves a thorough evaluation that includes a medical history review, physical examination, and specific tests to evaluate strength, range of motion, and functional abilities. This process allows the physical therapist to identify the underlying issues, set treatment goals, and develop a personalized rehabilitation plan. It also helps in monitoring progress throughout the treatment.
19. What role does patient education play in physical therapy?
Patient education is crucial in physical therapy as it empowers patients to understand their conditions, treatment options, and the importance of adherence to prescribed exercises and lifestyle modifications. Educating patients about injury prevention and self-management strategies fosters independence and promotes long-term health outcomes. Effective communication enhances the therapeutic relationship and encourages patient engagement in their recovery process.
20. What are some common conditions treated by physical therapists?
- Musculoskeletal Disorders: Conditions such as arthritis, back pain, and sports injuries.
- Neurological Disorders: Rehabilitation for stroke, multiple sclerosis, and Parkinson’s disease.
- Pediatric Conditions: Treatment for developmental delays, cerebral palsy, and other childhood disorders.
- Cardiopulmonary Conditions: Rehabilitation for heart and lung issues, enhancing endurance and functional capacity.
Physical therapists are trained to handle a wide range of conditions, and their interventions can significantly improve patients’ overall health and functionality.
21. What is the importance of setting SMART goals in physical therapy?
Setting SMART goals—Specific, Measurable, Achievable, Relevant, and Time-bound—is important in physical therapy as it provides a clear framework for treatment objectives. This approach ensures that both the therapist and patient have a mutual understanding of the expected outcomes and timelines. SMART goals facilitate progress tracking and adjustments to the treatment plan, helping to maintain motivation and focus on recovery.
Physical Therapist Intermediate Interview Questions
This section contains intermediate-level interview questions for Physical Therapists, focusing on practical applications, best practices, and real-world scenarios. Candidates should be familiar with patient assessment techniques, treatment planning, and rehabilitation strategies to excel in these interviews.
22. What are the key components of a comprehensive patient assessment in physical therapy?
A comprehensive patient assessment includes several key components, such as:
- Patient history: Collecting detailed information about the patient’s medical, surgical, and social history.
- Physical examination: Conducting a thorough evaluation of the patient’s physical condition, including range of motion, strength, and mobility.
- Functional assessment: Assessing the patient’s ability to perform daily activities and identifying any limitations.
- Goals setting: Collaborating with the patient to establish realistic and measurable treatment goals.
This holistic approach ensures a tailored treatment plan that addresses the patient’s specific needs.
23. How do you determine the appropriate treatment plan for a patient?
Determining an appropriate treatment plan involves several steps:
- Assessment findings: Analyze the results of the patient assessment to identify impairments and functional limitations.
- Evidence-based practice: Utilize current research and clinical guidelines to inform treatment choices.
- Patient preferences: Consider the patient’s personal goals and preferences to enhance adherence to the treatment plan.
- Progress monitoring: Regularly evaluate the patient’s progress and adjust the treatment plan as necessary.
Combining these elements leads to effective and individualized care.
24. What is the role of therapeutic exercises in rehabilitation?
Therapeutic exercises play a crucial role in rehabilitation by:
- Improving strength: Targeting specific muscle groups to enhance overall strength and endurance.
- Restoring range of motion: Facilitating joint mobility and flexibility through stretching and movement exercises.
- Enhancing balance and coordination: Incorporating balance training to prevent falls and improve functional stability.
- Promoting pain relief: Engaging in low-impact activities that can alleviate pain and promote healing.
These exercises are essential for helping patients regain independence and return to their daily activities.
25. How do you handle a patient who is non-compliant with their treatment plan?
Handling non-compliance requires effective communication and empathy. Here are some strategies:
- Understanding barriers: Discuss any obstacles the patient may face, such as pain, lack of understanding, or financial constraints.
- Education: Provide clear explanations of the importance of the treatment plan and the consequences of non-compliance.
- Goal setting: Collaboratively set achievable and realistic goals to motivate the patient.
- Regular follow-up: Maintain consistent communication to monitor progress and address concerns.
This approach fosters a trusting relationship and encourages patients to adhere to their treatment plans.
26. What techniques do you use for pain management in physical therapy?
Pain management techniques in physical therapy include:
- Manual therapy: Utilizing hands-on techniques to alleviate pain and improve mobility.
- Modalities: Applying heat, cold, ultrasound, or electrical stimulation to reduce pain and inflammation.
- Exercise prescription: Designing specific exercises that promote pain relief and enhance function.
- Patient education: Teaching patients about pain mechanisms and self-management strategies.
These techniques can be combined to create a comprehensive pain management strategy tailored to the individual patient.
27. Can you explain the significance of evidence-based practice in physical therapy?
Evidence-based practice (EBP) is significant in physical therapy for several reasons:
- Improved outcomes: EBP integrates the best available research with clinical expertise and patient values, leading to more effective treatment plans.
- Standardization of care: Utilizing established guidelines ensures consistency in treatment approaches across practitioners.
- Quality improvement: Regularly updating practices based on new research fosters continual improvement in patient care.
- Informed decision-making: EBP empowers therapists to make informed clinical decisions that align with the latest evidence.
Incorporating EBP can significantly enhance the quality of care provided to patients.
28. What are some common challenges you face when working with geriatric patients?
Common challenges when working with geriatric patients include:
- Multiple comorbidities: Managing various health conditions that can complicate treatment plans.
- Cognitive impairments: Addressing issues such as dementia or confusion that may impact communication and understanding.
- Reduced mobility: Working with patients who have decreased strength and endurance can limit exercise options.
- Motivational factors: Engaging elderly patients who may feel discouraged about their condition or progress.
Awareness of these challenges allows therapists to adapt their approaches and provide optimal care.
29. How do you incorporate patient education into your treatment sessions?
Incorporating patient education is essential for successful treatment outcomes. Strategies include:
- Demonstrating exercises: Showing patients how to perform exercises correctly to prevent injury and ensure effectiveness.
- Explaining conditions: Providing information about their diagnosis and treatment options to enhance understanding.
- Discussing home programs: Educating patients on exercises they can perform at home to maintain progress.
- Encouraging questions: Creating an open dialogue where patients feel comfortable asking about their treatment.
This empowers patients to take an active role in their recovery process.
30. What is the importance of interdisciplinary collaboration in physical therapy?
Interdisciplinary collaboration is crucial in physical therapy due to:
- Holistic care: Combining expertise from various disciplines leads to comprehensive care addressing all aspects of a patient’s health.
- Improved communication: Facilitating better communication between healthcare professionals reduces the risk of mismanagement.
- Shared knowledge: Learning from colleagues in different fields can enhance treatment strategies and approaches.
- Coordinated treatment plans: Ensuring that all team members are aligned with the patient’s goals optimizes care delivery.
This collaboration ultimately leads to better patient outcomes and satisfaction.
31. How do you evaluate a patient’s progress during therapy?
Evaluating a patient’s progress involves:
- Regular assessments: Conducting objective evaluations at different stages to measure improvements in strength, range of motion, and function.
- Patient feedback: Gathering subjective input from patients regarding their pain levels and perceived limitations.
- Goal review: Comparing progress against established treatment goals to determine if adjustments are necessary.
- Outcome measures: Utilizing standardized assessments to quantify progress and inform treatment decisions.
These methods ensure that the treatment remains effective and responsive to the patient’s needs.
32. What strategies do you use to prevent injuries in patients during rehabilitation?
Preventing injuries during rehabilitation involves several proactive strategies:
- Proper assessment: Identifying risk factors and pre-existing conditions that may increase injury risk.
- Individualized programs: Tailoring rehabilitation exercises to each patient’s abilities and limitations.
- Technique education: Teaching proper body mechanics and exercise techniques to avoid strain.
- Gradual progression: Slowly increasing the intensity and complexity of exercises to allow the body to adapt.
Implementing these strategies significantly reduces the likelihood of injury during the rehabilitation process.
33. How do you stay updated with the latest developments in physical therapy?
Staying updated with the latest developments in physical therapy is essential for providing high-quality care. Strategies include:
- Continuing education: Participating in workshops, courses, and conferences to enhance knowledge and skills.
- Research journals: Reading peer-reviewed journals to stay informed about emerging studies and evidence-based practices.
- Professional networks: Engaging with professional organizations and networks for access to resources and discussions.
- Online platforms: Following credible online platforms and forums where professionals share insights and experiences.
This commitment to lifelong learning ensures therapists remain effective and knowledgeable in their practice.
These intermediate-level questions are designed for physical therapy candidates to assess their knowledge in practical applications, best practices, and real-world scenarios in the field.
37. What are the key components of a comprehensive physical therapy assessment?
A comprehensive physical therapy assessment includes several key components: patient history, physical examination, evaluation of functional mobility, assessment of pain levels, and identification of goals. The patient history provides background information on the condition and lifestyle, while the physical examination involves tests for strength, range of motion, and balance. Functional mobility assessments gauge the patient’s ability to perform daily activities, and pain assessments help tailor treatment plans. Finally, setting achievable goals with the patient ensures a focused therapy approach.
38. How do you determine the appropriate treatment plan for a patient?
Determining an appropriate treatment plan involves a multi-step process: first, assessing the patient’s specific needs and goals; second, reviewing clinical findings and diagnostic information; third, considering evidence-based practices and guidelines; and finally, collaborating with the patient to incorporate their preferences and lifestyle. Treatment plans should be individualized, taking into account the patient’s age, activity level, and any comorbidities, and should include measurable objectives to track progress.
39. What role does patient education play in physical therapy?
Patient education is crucial in physical therapy for several reasons:
- Empowerment: Educating patients about their conditions and treatment options helps them take an active role in their recovery.
- Adherence: When patients understand the rationale behind exercises and therapies, they are more likely to follow through with their treatment plans.
- Prevention: Educating patients on proper body mechanics and injury prevention strategies can reduce the risk of future injuries.
- Self-management: Teaching patients techniques to manage their symptoms can lead to improved outcomes and independence.
Overall, effective patient education enhances engagement and encourages a successful recovery process.
40. Can you explain the significance of evidence-based practice in physical therapy?
Evidence-based practice (EBP) is significant in physical therapy as it ensures that treatment approaches are grounded in the best available research, clinical expertise, and patient values. EBP helps therapists make informed decisions, leading to better patient outcomes and improved quality of care. It allows practitioners to stay updated on the latest techniques and interventions, ensuring they apply the most effective methods. Furthermore, EBP facilitates accountability and supports the profession’s credibility by demonstrating the effectiveness of physical therapy interventions.
41. What strategies do you use to manage difficult patients in physical therapy?
Managing difficult patients requires a combination of communication skills and empathy. Here are some strategies:
- Active Listening: Understanding the patient’s concerns and frustrations can help build trust and rapport.
- Setting Clear Expectations: Clearly communicating the goals and processes of therapy can reduce anxiety and resistance.
- Flexibility: Adapting treatment plans to accommodate patient preferences or limitations can enhance cooperation.
- Encouragement: Providing positive reinforcement can motivate patients and improve their experience.
By employing these strategies, therapists can improve patient relationships and foster a more cooperative therapeutic environment.
42. How do you assess progress in a patient during physical therapy?
Assessing progress in a patient involves both subjective and objective measures:
- Subjective Measures: Regularly asking patients about their pain levels, functional abilities, and satisfaction with therapy provides insight into their progress.
- Objective Measures: Utilizing standardized tests and outcome measures, such as strength assessments, range of motion tests, and functional mobility scales, allows for quantifiable tracking of improvement.
- Goal Review: Comparing current performance against previously set goals helps determine if the patient is on track.
Regular reassessment ensures that treatment plans can be adjusted as necessary to meet the evolving needs of the patient.
Physical Therapist Interview Questions for Experienced
This section covers advanced interview questions for experienced Physical Therapists, focusing on complex treatment strategies, patient management, leadership skills, and the application of evidence-based practices. Candidates should be prepared to discuss their clinical reasoning, mentorship experiences, and approaches to optimizing patient care.
43. Can you describe a time when you had to adapt your treatment plan for a patient with unique needs?
In my experience, I once had a patient with a rare neurological condition that affected their mobility. I had to adapt the treatment plan by incorporating specialized exercises focusing on neuromuscular re-education and balance training. Collaborating with a multidisciplinary team helped in creating a comprehensive approach, ensuring the patient’s unique needs were met while promoting their independence.
44. What evidence-based practices do you incorporate into your treatment plans?
- Utilization of systematic reviews and clinical guidelines to inform practice.
- Incorporating patient-reported outcomes to tailor individualized care.
- Regularly updating my knowledge through continuing education and research to remain current with evolving best practices.
By integrating these evidence-based practices, I ensure that my treatment plans are not only effective but also aligned with the latest research in physical therapy.
45. How do you handle conflicts with colleagues regarding patient care?
Handling conflicts requires open communication and a focus on the patient’s best interest. I typically approach the situation by discussing my perspective with the colleague involved, seeking to understand their viewpoint as well. If necessary, I involve a supervisor to mediate the discussion, ensuring that the resolution remains patient-centered while preserving professional relationships.
46. Describe your experience with mentoring junior physical therapists.
I have mentored several junior physical therapists by providing guidance on clinical skills, treatment strategies, and professional development. I facilitate regular feedback sessions, encourage them to ask questions, and support them in case discussions. This mentorship has not only helped them build confidence but has also enhanced my leadership skills and reinforced my understanding of best practices.
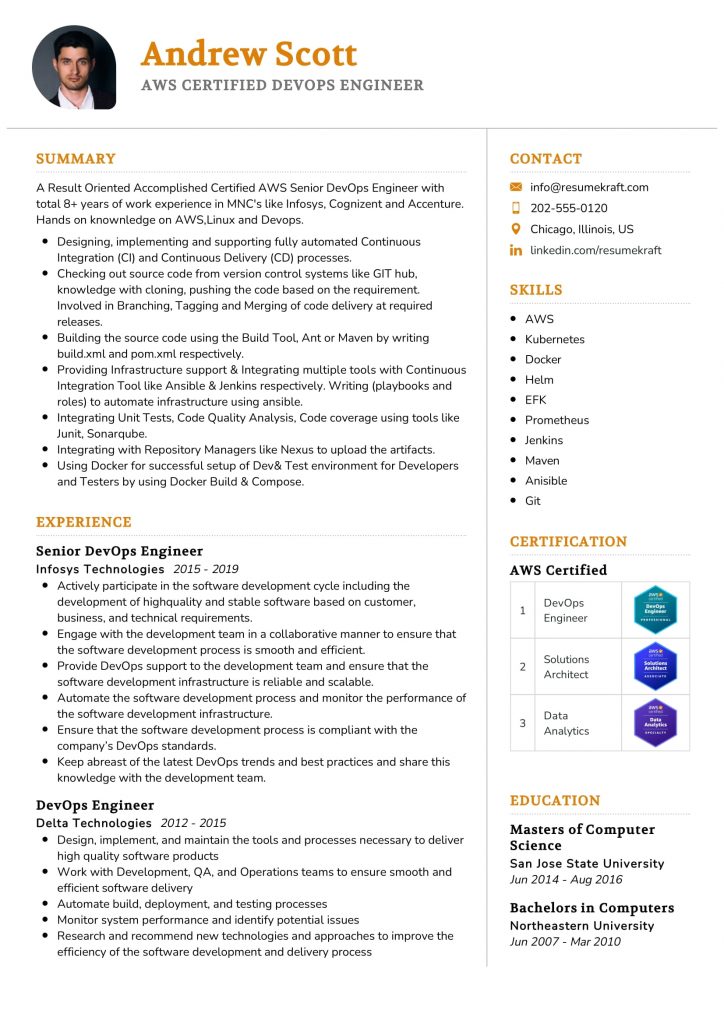
Build your resume in 5 minutes
Our resume builder is easy to use and will help you create a resume that is ATS-friendly and will stand out from the crowd.
47. How do you assess a patient’s progress and modify their treatment plan accordingly?
- Regular assessments using standardized outcome measures to track progress.
- Engaging patients in self-reported feedback to understand their perceptions of improvement.
- Adjusting treatment strategies based on the patient’s response and adherence to the plan.
This dynamic assessment process allows me to adapt treatment plans effectively, ensuring they remain relevant and effective for the patient’s evolving needs.
48. What role does technology play in your physical therapy practice?
Technology plays a significant role in enhancing patient care and outcomes. I utilize electronic health records for tracking progress, telehealth platforms for remote consultations, and specialized software for exercise prescriptions. Additionally, I stay updated on emerging technologies, such as virtual reality and gamification, which can enhance patient engagement and motivation during rehabilitation.
49. Can you discuss a time when you had to lead a team in a challenging situation?
During a particularly busy period at the clinic, I was asked to lead a team managing an influx of new patients. I organized daily briefings to prioritize cases, delegated tasks based on individual strengths, and ensured clear communication. This collaborative approach not only helped us manage the workload effectively but also fostered team cohesion and improved patient care during a challenging time.
50. What strategies do you use to stay updated with the latest research in physical therapy?
- Joining professional organizations that provide access to journals and conferences.
- Participating in webinars and workshops focusing on recent advancements.
- Engaging in discussions with peers and utilizing social media platforms to share insights.
By employing these strategies, I ensure I remain informed about the latest developments, which I then apply to improve my practice.
51. How do you ensure patient safety during treatments?
Ensuring patient safety is my top priority. I conduct thorough assessments before starting any treatment, maintain clear communication with patients about their conditions, and continuously monitor their responses during therapy sessions. I also stay updated on safety protocols and guidelines to minimize risks and prevent any potential complications during treatments.
52. Describe a particularly difficult case you managed and the outcome.
One of my most challenging cases involved a patient recovering from a complex orthopedic surgery. The patient had significant pain and limited mobility. I employed a combination of manual therapy, pain management techniques, and a gradual exercise program tailored to their needs. Over time, the patient made substantial progress, regaining mobility and reducing pain, which was highly rewarding for both of us.
53. What are the key considerations when developing a rehabilitation program for athletes?
- Assessing the specific nature and extent of the injury to tailor the program.
- Considering the athlete’s sport-specific demands and recovery timeline.
- Incorporating strength, flexibility, and functional training to ensure return-to-play readiness.
By addressing these considerations, I can create a comprehensive rehabilitation program that optimally supports the athlete’s recovery and performance goals.
54. How do you approach interdisciplinary collaboration in patient care?
I prioritize open communication and mutual respect when collaborating with other healthcare professionals. Regular interdisciplinary meetings to discuss patient cases allow us to share insights and develop cohesive treatment plans. I also believe in involving the patient in discussions, ensuring they understand the collaborative approach to their care and encouraging their active participation in the treatment process.
55. What methods do you use for patient education and engagement during therapy?
- Utilizing visual aids and demonstrations to enhance understanding of exercises.
- Incorporating patient goals into the treatment plan to increase motivation.
- Providing written materials and resources for patients to review at home.
These methods help ensure that patients are well-informed and engaged in their therapy, ultimately leading to improved outcomes and adherence to the treatment plan.
The following are advanced interview questions tailored for experienced Physical Therapists, focusing on their expertise in patient care, treatment methodologies, and professional development.
58. How do you approach creating a treatment plan for a patient with chronic pain?
Creating a treatment plan for a patient with chronic pain requires a comprehensive assessment and a patient-centered approach. Key steps include:
- Initial Assessment: Conduct a thorough evaluation of the patient’s medical history, pain levels, and functional limitations.
- Goal Setting: Collaborate with the patient to establish realistic and achievable goals that focus on pain reduction and improving function.
- Intervention Selection: Choose appropriate interventions, such as therapeutic exercises, manual therapy, and education on pain management strategies.
- Progress Monitoring: Regularly assess the patient’s progress and adjust the treatment plan as needed to ensure continued improvement.
This tailored approach helps address the unique needs of each patient and fosters a collaborative therapeutic relationship.
59. Can you discuss the importance of evidence-based practice in Physical Therapy?
Evidence-based practice (EBP) is crucial in Physical Therapy as it ensures that treatment decisions are grounded in the best available research, clinical expertise, and patient preferences. The importance of EBP includes:
- Improved Outcomes: Utilizing EBP leads to better patient outcomes by employing interventions that have been scientifically validated.
- Enhanced Decision-Making: EBP empowers therapists to make informed decisions tailored to individual patient needs, improving the quality of care.
- Professional Development: Engaging with current research fosters continuous learning and keeps practitioners updated on the latest methodologies.
Overall, EBP is essential for advancing the field of Physical Therapy and ensuring high standards of patient care.
60. How do you mentor new Physical Therapists in your practice?
Mentoring new Physical Therapists is vital for professional growth and enhancing team dynamics. My mentoring approach includes:
- Structured Onboarding: Provide a comprehensive orientation that covers clinical protocols, patient management techniques, and workplace culture.
- Regular Check-Ins: Schedule consistent meetings to discuss challenges, progress, and provide constructive feedback, fostering an open communication environment.
- Shadowing Opportunities: Allow new therapists to observe my treatment sessions to learn practical skills and patient interaction strategies.
- Encouraging Continued Education: Motivate mentees to pursue advanced training and attend workshops, reinforcing the importance of lifelong learning in our field.
This structured mentoring framework not only supports the professional development of new therapists but also enhances the overall quality of care provided within the practice.
How to Prepare for Your Physical Therapist Interview
Preparing for a Physical Therapist interview requires a blend of clinical knowledge, interpersonal skills, and a deep understanding of patient care. The following tips will help you effectively showcase your qualifications and readiness for the role.
Research the facility where you’re interviewing. Understand its mission, values, and the patient demographics it serves. This knowledge can help you tailor your responses and demonstrate your genuine interest in contributing to their team.
Review common physical therapy techniques and recent advancements in the field. Be prepared to discuss how you would apply these techniques in practice. This shows your commitment to continuing education and your readiness to implement evidence-based practices.
Practice answering behavioral interview questions using the STAR method (Situation, Task, Action, Result). Prepare examples from your clinical rotations or experiences that highlight your problem-solving skills and ability to work in a team.
Prepare questions to ask your interviewers about their practices and expectations. Inquiring about their approach to patient care or professional development opportunities demonstrates your enthusiasm and foresight in your career.
Dress professionally and appropriately for the interview. A polished appearance not only boosts your confidence but also reflects your respect for the profession and the interviewers. Choose comfortable yet formal attire suitable for a healthcare setting.
Bring copies of your resume, certifications, and any relevant documentation. Being organized will help you feel more confident and allows you to provide proof of your qualifications when discussing your experiences and skills.
Consider a mock interview with a mentor or a peer. This allows you to practice your responses and receive constructive feedback. A mock interview can help mitigate anxiety and improve your delivery during the actual interview.
Common Physical Therapist Interview Mistakes to Avoid
When interviewing for a Physical Therapist position, it’s crucial to present yourself professionally and effectively. Avoiding common mistakes can significantly enhance your chances of success and demonstrate your qualifications for the role.
- Failing to Research the Facility: Not understanding the facility’s mission, values, and patient demographics can make you appear unprepared and disinterested. Researching beforehand shows your commitment and helps tailor your responses.
- Neglecting to Prepare for Behavioral Questions: Many interviews include behavioral questions. Failing to prepare specific examples of past experiences can hinder your ability to demonstrate your skills and problem-solving abilities effectively.
- Overlooking the Importance of Soft Skills: Physical therapy requires excellent communication, empathy, and teamwork. Focusing solely on technical skills may lead you to neglect discussing your interpersonal abilities, which are equally important.
- Not Asking Questions: Interviews are a two-way street. Failing to ask insightful questions about the role or the team can signal a lack of interest in the position or the organization.
- Being Vague About Your Experience: When discussing your past roles, be specific about your responsibilities and achievements. Vague answers can make it difficult for interviewers to gauge your qualifications and fit.
- Underestimating the Importance of Dress Code: Dressing too casually for the interview can convey a lack of professionalism. Choose appropriate attire that reflects the work environment and shows respect for the interview process.
- Not Practicing Your Responses: Going into an interview without practicing your answers can lead to stumbling over words or failing to articulate key points. Mock interviews can help you convey your thoughts clearly and confidently.
- Failing to Follow Up: Not sending a thank-you note or email after the interview can be a missed opportunity to express gratitude and reinforce your interest in the position. A follow-up can leave a lasting positive impression.
Key Takeaways for Physical Therapist Interview Success
- Prepare a tailored resume using effective resume templates to highlight your relevant experience and skills. Consider utilizing an AI resume builder for enhanced formatting and structure.
- Showcase your clinical experience by including concrete resume examples that demonstrate your impact in previous roles, emphasizing patient outcomes and rehabilitation success stories.
- Craft compelling cover letters that reflect your passion for physical therapy and align your values with the organization’s mission to create a strong first impression.
- Engage in mock interview practice to refine your communication skills and boost your confidence, ensuring you articulate your qualifications clearly during the actual interview.
- Research the employer thoroughly to ask insightful questions during the interview, showing your genuine interest in the position and understanding of the company’s approach to patient care.
Frequently Asked Questions
1. How long does a typical Physical Therapist interview last?
A typical Physical Therapist interview lasts between 30 minutes to an hour. This duration allows the interviewer to assess your clinical knowledge, communication skills, and cultural fit within the organization. Be prepared for questions about your experience, treatment approaches, and patient interactions. Additionally, some interviews may include a practical component or role-playing scenario, which could extend the time. It’s essential to be concise yet thorough in your responses to make a positive impression.
2. What should I wear to a Physical Therapist interview?
For a Physical Therapist interview, aim for professional attire that reflects your seriousness about the role. Business casual is typically appropriate; consider wearing slacks or a knee-length skirt with a collared shirt or blouse. Closed-toe shoes are recommended, as they maintain a professional appearance. Avoid overly casual clothing, such as jeans or sneakers, to convey your respect for the interview process. Bright colors are acceptable, but keep the overall look polished and neat.
3. How many rounds of interviews are typical for a Physical Therapist position?
Typically, the interview process for a Physical Therapist position may involve two to three rounds. The first round is often a phone or video interview focusing on your background and qualifications. Subsequent rounds may include in-person interviews, where you’ll meet with potential colleagues or supervisors to discuss clinical skills and teamwork. Some facilities may also include a practical evaluation. Each round is an opportunity to demonstrate your expertise and fit for the role.
4. Should I send a thank-you note after my Physical Therapist interview?
Yes, sending a thank-you note after your Physical Therapist interview is highly recommended. It shows appreciation for the interviewer’s time and reinforces your interest in the position. In your note, briefly mention specific topics discussed during the interview that resonated with you, which helps personalize your message. Aim to send this note within 24 hours, either via email or traditional mail, depending on the company’s culture. A thoughtful thank-you can leave a lasting impression.