Preparing for a Physician Assistant (PA) interview is a crucial step in your journey towards a rewarding career in healthcare. The PA role is unique as it combines medical knowledge with patient care, requiring strong communication skills and the ability to work collaboratively within a team. Given the competitive nature of PA programs and the increasing demand for healthcare professionals, proper interview preparation is essential to showcase your qualifications and passion for the field. This comprehensive guide will cover common interview questions, effective strategies for presenting your experience, tips for highlighting your interpersonal skills, and insights into what interviewers look for in a successful candidate.
What to Expect in a Physician Assistant Interview
In a Physician Assistant interview, candidates can expect a structured format that may include multiple interviewers, such as physicians, PAs, and admissions staff. The interview process typically consists of behavioral questions, clinical scenarios, and discussions about the candidate’s experience and motivation for pursuing the PA profession. Candidates should be prepared for both one-on-one and panel interviews, where they will be assessed on their clinical knowledge, teamwork skills, and ability to handle challenging situations. Overall, the interview aims to evaluate both technical competencies and interpersonal skills essential for patient care.
Physician Assistant Interview Questions For Freshers
Preparing for a Physician Assistant interview requires a solid grasp of essential medical knowledge, patient care practices, and the ability to communicate effectively. Freshers should focus on mastering fundamental concepts such as medical ethics, clinical procedures, and interpersonal skills to excel in their interviews.
1. What is the role of a Physician Assistant?
A Physician Assistant (PA) is a licensed medical professional who practices medicine under the supervision of a physician. PAs perform various duties, including taking medical histories, conducting physical exams, diagnosing illnesses, developing treatment plans, and prescribing medications. They play a crucial role in providing patient care and improving healthcare access.
2. What are the educational requirements to become a Physician Assistant?
To become a Physician Assistant, one must complete a master’s degree from an accredited PA program. This typically requires a bachelor’s degree, completion of healthcare-related experience, and specific prerequisite courses. After graduation, candidates must pass the Physician Assistant National Certifying Exam (PANCE) to become licensed.
3. How do you handle stressful situations in a clinical setting?
- Stay Calm: Maintaining composure helps to think clearly and make better decisions.
- Prioritize Tasks: Focus on the most critical tasks first, ensuring patient safety.
- Seek Support: Collaborate with team members for assistance and share responsibility.
Handling stress effectively is crucial in clinical settings, as it ensures that you can provide the best care for patients even in challenging situations.
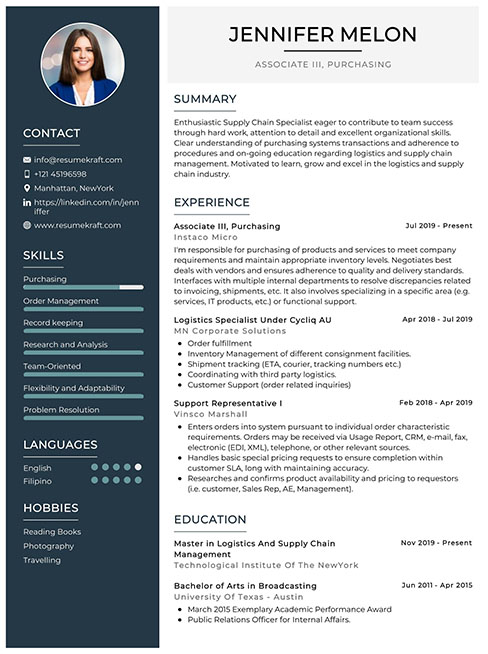
Build your resume in just 5 minutes with AI.
4. Can you explain the importance of patient confidentiality?
Patient confidentiality is vital in healthcare as it builds trust between patients and providers. It ensures that personal health information is protected, fosters open communication, and is mandated by laws such as HIPAA. Violating confidentiality can lead to legal consequences and a loss of patient trust.
5. What are some common challenges faced by Physician Assistants?
- Scope of Practice: Understanding the legal limitations of their practice can be challenging.
- Workload: Managing high patient volumes and varied cases can lead to burnout.
- Collaboration: Effectively communicating and collaborating with physicians and other healthcare professionals is essential.
Being aware of these challenges helps PAs prepare to navigate their roles effectively and improve patient care.
6. How do you ensure accurate patient assessments?
Accurate patient assessments require careful attention to detail, effective communication with patients, and thorough physical examinations. Utilizing standardized assessment tools and keeping up-to-date with clinical guidelines also enhances the accuracy of evaluations, ensuring patients receive the appropriate care and treatment.
7. Describe a time when you had to work as part of a team.
In a clinical setting, teamwork is essential for providing effective patient care. An example could involve collaborating with nurses and physicians to develop a comprehensive treatment plan for a patient with complex needs, ensuring that all team members contribute their expertise for the patient’s benefit.
8. What steps do you take to stay current with medical knowledge?
- Continuing Education: Attend workshops, seminars, and conferences.
- Professional Journals: Regularly read relevant medical journals and articles.
- Networking: Engage with other professionals to share knowledge and experiences.
Staying current with medical knowledge is crucial for delivering high-quality patient care and adapting to new treatments and technologies.
9. How do you approach patient education?
Patient education involves assessing the patient’s understanding, providing clear and concise information, and using teaching aids when necessary. Tailoring the education to the patient’s needs and ensuring they comprehend their condition and treatment options is essential for promoting adherence and improving outcomes.
10. What role does empathy play in patient care?
Empathy is crucial in patient care as it helps build rapport and trust between the provider and the patient. It allows PAs to understand patients’ feelings and concerns, which can lead to better communication, improved patient satisfaction, and more effective treatment plans tailored to individual needs.
11. Can you describe the process of diagnosing a patient?
- Gathering History: Collect detailed patient history and symptoms.
- Physical Examination: Conduct a thorough physical exam to identify signs.
- Diagnostic Tests: Order appropriate lab tests or imaging studies as needed.
- Analysis: Analyze the findings to arrive at a diagnosis.
The diagnostic process is systematic and ensures that all necessary information is considered before making a clinical decision.
12. How do you manage time effectively in a busy clinic?
Effective time management involves prioritizing tasks, using scheduling tools, and setting realistic goals for each patient visit. It’s essential to remain organized and maintain clear communication with the healthcare team to ensure that patient needs are met efficiently within the constraints of the clinic’s workload.
13. What is your experience with electronic health records (EHR)?
Electronic Health Records (EHR) are vital for modern healthcare, allowing for efficient documentation, patient tracking, and communication among providers. Familiarity with EHR systems enables PAs to streamline patient care, enhance accuracy in record-keeping, and improve overall workflow in clinical settings.
14. How do you handle difficult patients?
- Active Listening: Listen to the patient’s concerns without interruption.
- Stay Calm: Maintain professionalism and composure, even in challenging situations.
- Find Common Ground: Work towards a solution that addresses the patient’s concerns while ensuring appropriate care.
Handling difficult patients with empathy and professionalism can lead to better outcomes and improved patient relationships.
15. Why do you want to become a Physician Assistant?
The motivation to become a Physician Assistant often stems from a desire to help others and make a meaningful impact in the healthcare field. Many candidates are drawn to the role because of the opportunity to work closely with patients, collaborate with healthcare teams, and contribute to improving health outcomes.
These questions are designed for freshers entering the Physician Assistant field and cover fundamental concepts they should master.
16. What is the role of a Physician Assistant (PA)?
A Physician Assistant (PA) is a medical professional who practices medicine under the supervision of a physician. PAs are trained to perform a variety of tasks, including taking medical histories, conducting physical exams, diagnosing illnesses, and developing treatment plans. They also assist in surgeries, interpret diagnostic tests, and provide patient education. The role of a PA is crucial in improving patient access to healthcare and enhancing the efficiency of medical teams.
17. What are the educational requirements to become a Physician Assistant?
To become a Physician Assistant, candidates typically need to complete a master’s degree from an accredited PA program, which usually requires a bachelor’s degree and relevant healthcare experience as prerequisites. The curriculum includes coursework in anatomy, pharmacology, and clinical medicine, followed by clinical rotations in various medical specialties. After completing the program, candidates must pass the Physician Assistant National Certifying Exam (PANCE) to practice.
18. What is the difference between a PA and a Nurse Practitioner (NP)?
- Education: PAs typically attend a master’s-level program, while NPs often have advanced practice nursing degrees.
- Scope of Practice: PAs can work in various specialties without needing additional certification, while NPs often focus on a particular area of care.
- Supervision: PAs work under a physician’s supervision, whereas NPs can practice independently in many states.
Despite these differences, both roles are essential in providing high-quality patient care and can perform many similar functions.
19. Describe the typical workflow of a Physician Assistant in a clinical setting.
The workflow of a Physician Assistant generally begins with seeing patients, where they take medical histories and perform physical examinations. They then assess the patient’s condition, order diagnostic tests, and interpret the results. Following this, PAs collaborate with physicians to develop treatment plans and prescribe medications as needed. They also provide follow-up care, educate patients about their health conditions, and document all interactions in the medical record.
20. How do PAs handle patient education and counseling?
PAs play a vital role in patient education by explaining medical conditions, treatment options, and preventive measures in a way that is understandable. They assess the patient’s knowledge level, address any misconceptions, and ensure that patients are informed about their health decisions. Effective communication skills are essential, as PAs must be able to convey complex information clearly and empathetically, fostering a trusting relationship with patients.
21. What are some common challenges faced by Physician Assistants?
- Time Management: PAs often juggle multiple patients and tasks, requiring excellent time management skills to ensure quality care.
- Regulatory Changes: Staying updated with healthcare laws and regulations is crucial, as they can impact practice.
- Interprofessional Collaboration: PAs must navigate different team dynamics and communication styles while working with diverse healthcare professionals.
These challenges require PAs to be adaptable, resourceful, and committed to lifelong learning in the ever-evolving healthcare landscape.
22. What is the importance of continuing education for Physician Assistants?
Continuing education is vital for Physician Assistants to maintain their certification and stay abreast of the latest medical advancements, treatments, and technologies. It ensures that PAs can provide the highest quality of care and adapt to changes in clinical guidelines. Many states require PAs to complete a certain number of continuing education hours every two years, emphasizing the importance of ongoing professional development in this dynamic field.
23. How do PAs contribute to patient safety in healthcare settings?
PAs contribute to patient safety through thorough assessments, accurate documentation, and adherence to protocols. They actively participate in patient safety initiatives, including identifying potential risks and implementing preventive measures. PAs also engage in interdisciplinary communication, ensuring that all healthcare team members are informed about patient care plans, which helps in reducing errors and improving overall patient outcomes.
Physician Assistant Intermediate Interview Questions
Preparing for a Physician Assistant interview requires an understanding of mid-level concepts such as patient assessment, treatment planning, and healthcare regulations. Candidates should be ready to discuss practical applications, clinical scenarios, and best practices in patient care.
24. What are the key components of a comprehensive patient assessment?
A comprehensive patient assessment includes several key components: a detailed medical history, a thorough physical examination, and relevant diagnostic testing. Additionally, it involves evaluating the patient’s psychosocial environment and understanding their health beliefs and preferences. This holistic approach ensures that all aspects of the patient’s condition are considered in treatment planning.
25. How do you prioritize patient care in a busy clinical setting?
Prioritizing patient care in a busy clinical setting involves assessing the urgency of each patient’s needs based on their symptoms and medical history. Utilizing triage protocols, collaborating with the healthcare team, and effectively managing time are critical. It’s important to address life-threatening conditions first while ensuring that all patients receive appropriate care in a timely manner.
26. Explain the role of evidence-based practice in clinical decision-making.
Evidence-based practice (EBP) integrates the best available research, clinical expertise, and patient values in clinical decision-making. This approach involves critically appraising current literature to inform practice and improve patient outcomes. By utilizing EBP, Physician Assistants can provide high-quality care that is scientifically validated and tailored to individual patient needs.
27. What are common side effects of antibiotics, and how would you counsel a patient experiencing them?
- Gastrointestinal upset: Common side effects include nausea, vomiting, and diarrhea. Advise patients to take antibiotics with food to minimize these effects.
- Allergic reactions: Educate patients about signs of an allergic reaction, such as rash or difficulty breathing, and instruct them to seek immediate medical attention if these occur.
Providing thorough counseling ensures patients understand their treatment and can manage any side effects effectively.
28. Describe the importance of patient education in chronic disease management.
Patient education is crucial in chronic disease management as it empowers patients to understand their condition, treatment options, and self-management strategies. Educating patients about lifestyle modifications, medication adherence, and monitoring symptoms can lead to better health outcomes. It also fosters a collaborative relationship between the provider and the patient, enhancing adherence to treatment plans.
29. How do you handle a situation where a patient refuses treatment?
Handling a patient who refuses treatment requires empathy and effective communication. First, it’s important to understand the reasons behind their decision, whether they stem from fear, misunderstanding, or cultural beliefs. Providing clear, concise information about the benefits and risks of the treatment can help address concerns. Ultimately, respecting the patient’s autonomy while ensuring they are fully informed is critical.
30. What strategies can you implement to improve patient adherence to treatment plans?
- Clear communication: Ensure that patients understand their treatment plan, including medications and lifestyle changes.
- Follow-up support: Regular check-ins and follow-up appointments can help monitor progress and address any barriers to adherence.
- Involving family: Engaging family members can provide additional support and encouragement for the patient.
These strategies can lead to improved adherence and better health outcomes.
31. Explain the concept of cultural competence in healthcare.
Cultural competence involves understanding and respecting diverse cultural backgrounds and how they influence health beliefs and practices. It is essential for providing effective patient care, as it helps in building trust and rapport with patients. Culturally competent care includes being aware of language barriers, dietary preferences, and traditional healing practices, ensuring that care is tailored to individual patient needs.
32. What are the legal considerations a Physician Assistant must keep in mind when prescribing medications?
Legal considerations for prescribing medications include understanding state regulations regarding prescriptive authority, ensuring appropriate documentation in the patient’s medical record, and adhering to guidelines for controlled substances. PAs must also stay informed about drug interactions and contraindications, and they should provide thorough patient education on medication use and potential side effects to ensure compliance with legal standards.
33. How would you approach a situation where a colleague is not following protocol?
Addressing a colleague who is not following protocol requires a careful and professional approach. I would first verify the facts and then have a private conversation with the colleague to express my concerns. It’s important to discuss the potential implications for patient safety and care quality. If the behavior persists, I would consider escalating the issue to a supervisor to ensure that proper protocols are upheld.
34. Discuss the significance of maintaining patient confidentiality.
Maintaining patient confidentiality is vital for building trust and ensuring ethical practice. It is a legal requirement under laws such as HIPAA, which protects patient information. Breaches of confidentiality can harm the patient-provider relationship and lead to legal consequences. Therefore, it’s essential to practice discretion and safeguard patient information in all aspects of care.
35. What are some effective ways to conduct a patient follow-up?
- Phone calls: Directly contacting patients after treatment to check on their recovery and address any concerns.
- Telehealth: Utilizing virtual appointments for follow-ups to increase accessibility and convenience.
- Patient surveys: Sending questionnaires to gather feedback on their experience and outcomes.
These methods enhance patient engagement and can identify any ongoing issues that need addressing.
36. How do you stay updated with the latest medical guidelines and practices?
Staying updated with the latest medical guidelines involves regularly reading peer-reviewed journals, attending professional conferences, and participating in continuing education courses. Subscribing to reputable medical organizations and networking with colleagues can also provide insights into emerging practices and guidelines. This ongoing education is crucial for providing optimal patient care.
37. What role does teamwork play in a healthcare setting?
Teamwork in healthcare is essential for delivering high-quality patient care. It involves collaboration among various professionals, such as physicians, nurses, and allied health staff, to develop comprehensive treatment plans. Effective teamwork enhances communication, reduces errors, and improves patient outcomes by leveraging the diverse expertise of team members to address complex health issues.
38. Describe a challenging case you encountered and how you managed it.
In one challenging case, I encountered a patient with multiple comorbidities who was non-compliant with medications. I managed it by conducting a thorough assessment to understand the barriers to adherence. I then developed a tailored education plan addressing their concerns and simplified their medication regimen. Regular follow-ups helped them gradually improve their adherence and health outcomes.
Here are some intermediate-level interview questions designed for Physician Assistant candidates. These questions focus on practical applications, clinical scenarios, and essential skills relevant to the role.
39. How do you approach a patient with suspected diabetes mellitus?
When approaching a patient with suspected diabetes mellitus, I would begin with a comprehensive assessment that includes a detailed medical history and physical examination. Important steps include:
- Screening for classic symptoms: I would inquire about polyuria, polydipsia, and unexplained weight loss.
- Laboratory tests: I would order fasting plasma glucose, HbA1c, or an oral glucose tolerance test to confirm the diagnosis.
- Patient education: Discussing lifestyle modifications, dietary changes, and the importance of regular follow-up is essential.
This holistic approach ensures proper diagnosis and management aimed at improving patient outcomes.
40. What are the key components of a physical examination for a patient presenting with chest pain?
A thorough physical examination for a patient with chest pain should include the following key components:
- Vital signs: Monitoring blood pressure, heart rate, respiratory rate, and temperature.
- Inspection: Observing for distress, cyanosis, or diaphoresis.
- Pulses: Checking peripheral pulses for symmetry and strength.
- Cardiovascular assessment: Auscultating heart sounds for murmurs or abnormal rhythms.
- Respiratory assessment: Listening for abnormal lung sounds such as wheezing or crackles.
This comprehensive evaluation aids in identifying potential life-threatening conditions and guiding further diagnostic testing.
41. Describe a time when you had to manage a difficult patient interaction.
In a previous role, I encountered a patient who was upset about a long wait time. I approached the situation by first listening to their concerns without interrupting. I acknowledged their frustration and apologized for the inconvenience. I then explained the reason for the delay and offered to provide updates while they waited. By addressing their feelings and maintaining open communication, I was able to de-escalate the situation and restore trust, which ultimately improved their experience.
42. What are the most common side effects of antibiotics, and how do you counsel patients about them?
Common side effects of antibiotics include:
- Diarrhea: Often due to disruption of gut flora; I advise patients to stay hydrated and inform me if it persists.
- Nausea and vomiting: Counseling on taking antibiotics with food can help mitigate these symptoms.
- Allergic reactions: I emphasize the importance of recognizing signs of an allergic reaction, such as rash or difficulty breathing, and to seek immediate medical attention if these occur.
Proper counseling helps patients understand potential side effects and encourages adherence to the prescribed treatment.
43. How do you prioritize patient care in a busy clinical setting?
In a busy clinical setting, prioritizing patient care involves assessing the urgency of each case based on clinical guidelines. I typically follow these steps:
- Triage: Quickly evaluating patients to determine who requires immediate attention based on severity and potential complications.
- Time management: Allocating appropriate time slots for each patient while being flexible to accommodate urgent cases.
- Team communication: Collaborating with other healthcare professionals to ensure that all patients receive timely care.
This structured approach helps maintain high-quality care even during peak times.
44. Explain the importance of documentation in patient care.
Documentation in patient care is crucial for several reasons:
- Legal protection: Accurate records protect healthcare providers in case of disputes or legal issues.
- Continuity of care: Well-documented notes ensure that all team members are informed about a patient’s history, treatment plans, and changes in condition.
- Quality assurance: Documentation allows for the monitoring of patient outcomes and adherence to clinical guidelines, ultimately improving care quality.
Therefore, thorough and precise documentation is essential for effective and safe patient management.
45. What strategies do you use to stay current with medical knowledge and practices?
To stay current with medical knowledge and practices, I employ several strategies:
- Continuous education: I participate in workshops and conferences related to my field to learn about the latest advancements.
- Professional journals: I regularly read peer-reviewed journals to stay informed about new research and clinical guidelines.
- Networking: Engaging with colleagues and joining professional organizations provides insights into best practices and emerging trends.
These strategies help ensure that my knowledge remains up-to-date, ultimately benefiting my patients.
Physician Assistant Interview Questions for Experienced
This section focuses on interview questions tailored for experienced Physician Assistants. It covers advanced topics such as clinical decision-making, patient management strategies, leadership roles, and the implementation of evidence-based practices in healthcare settings.
47. How do you approach clinical decision-making in complex cases?
In complex clinical cases, I utilize a systematic approach that includes thorough patient assessment, collaboration with interdisciplinary teams, and evidence-based guidelines. I prioritize gathering comprehensive patient history and conducting diagnostic tests, followed by evaluating treatment options and potential outcomes. This method ensures that I provide well-informed care while considering the patient’s unique circumstances and preferences.
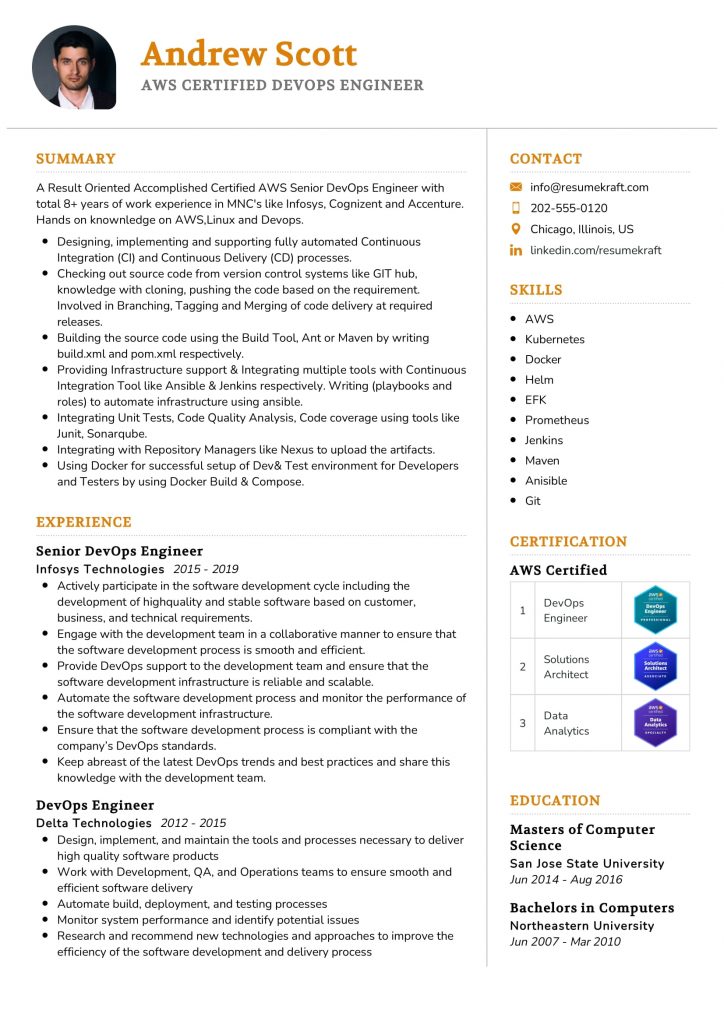
Build your resume in 5 minutes
Our resume builder is easy to use and will help you create a resume that is ATS-friendly and will stand out from the crowd.
48. Can you describe your experience with electronic health record (EHR) optimization?
I have led initiatives to optimize EHR systems by streamlining workflows and enhancing user interfaces. This included training staff on best practices, implementing standardized templates for common conditions, and utilizing data analytics to identify areas for improvement. This optimization not only increased efficiency but also improved patient documentation and communication across the healthcare team.
49. What strategies do you employ to mentor junior Physician Assistants?
- Regular One-on-One Meetings: I schedule consistent check-ins to discuss their progress, address concerns, and provide guidance.
- Hands-On Training: I involve them in patient cases to develop their clinical skills and decision-making abilities.
- Encouraging Continuing Education: I promote attending workshops and conferences to keep them updated on the latest practices.
This mentorship approach fosters a supportive learning environment and accelerates their professional growth.
50. How do you manage patient load during peak hours?
During peak hours, I prioritize effective time management and delegation. I assess the urgency of cases and triage patients accordingly. Utilizing a team-based approach, I delegate tasks to nursing staff and collaborate with other healthcare providers to ensure timely care. Additionally, I employ efficient documentation practices to minimize time spent on administrative tasks.
51. Describe a time when you had to implement a new protocol. How did you handle it?
When implementing a new diabetes management protocol, I first gathered the team to discuss the rationale and benefits. I provided training sessions to ensure everyone understood the new guidelines and their roles. By incorporating feedback and fostering an open dialogue, we were able to smoothly transition to the new protocol, resulting in improved patient outcomes and satisfaction.
52. What role does evidence-based practice play in your patient care?
Evidence-based practice is fundamental to my approach to patient care. I consistently review current literature and clinical guidelines to inform my decisions. By integrating the best available evidence with clinical expertise and patient values, I ensure that the care I provide is both effective and aligned with the latest standards, ultimately enhancing patient outcomes.
53. How do you handle conflicts within a healthcare team?
In handling conflicts, I prioritize open communication and active listening. I encourage team members to express their perspectives while facilitating a respectful dialogue. By focusing on the common goal of patient care, I help mediate discussions and find mutually agreeable solutions. This approach fosters a collaborative environment and strengthens team dynamics.
54. Can you provide an example of a successful patient outcome you facilitated?
One successful outcome involved a patient with chronic obstructive pulmonary disease (COPD) who was frequently hospitalized. I developed a comprehensive care plan that included medication management, lifestyle modifications, and regular follow-ups. By closely monitoring the patient’s progress and adjusting the treatment plan as needed, we significantly reduced hospital visits and improved their quality of life.
55. How do you ensure compliance with regulatory standards in your practice?
- Regular Training: I conduct training sessions for the team on updates in healthcare regulations and compliance requirements.
- Audits and Assessments: I perform regular audits of our practices to identify areas of non-compliance and address them promptly.
- Staying Informed: I keep abreast of changes in laws and regulations to ensure our protocols remain compliant.
This proactive approach minimizes risks and ensures that we provide safe and effective care.
56. What techniques do you use to build rapport with patients?
I build rapport with patients through active listening, showing empathy, and maintaining a non-judgmental attitude. I take the time to understand their concerns and preferences, which fosters trust and encourages open communication. Additionally, I ensure that I explain medical terms in layman’s language, making the patient feel more comfortable and engaged in their care.
57. How do you stay current with advancements in medical knowledge and practices?
I stay current by regularly attending medical conferences, participating in online courses, and subscribing to relevant medical journals. Networking with other professionals and engaging in discussion forums also provides insights into the latest developments. This continuous learning approach ensures that I remain informed and can apply the best practices in my clinical work.
58. Describe your experience in managing chronic diseases.
My experience in managing chronic diseases includes developing individualized care plans, coordinating with specialists, and providing patient education. I focus on monitoring disease progression, adjusting treatment regimens, and motivating patients to adhere to their plans. This comprehensive management approach has led to improved health outcomes and enhanced quality of life for my patients.
59. How do you approach cultural competence in patient care?
I approach cultural competence by actively seeking to understand the diverse backgrounds of my patients. I engage in training on cultural sensitivity and adapt my communication styles to meet the needs of different populations. This includes being aware of cultural beliefs surrounding health and illness, which helps me provide more personalized and respectful care.
60. What leadership qualities do you consider most important in a Physician Assistant?
- Effective Communication: The ability to clearly convey information and listen to team members.
- Empathy: Understanding and addressing the emotional needs of both patients and staff.
- Decision-Making: Being able to make informed and timely decisions in a clinical setting.
These qualities are essential for fostering a positive work environment and ensuring high-quality patient care.
Here are some experienced interview questions tailored for Physician Assistants, focusing on critical aspects of their role in healthcare.
62. How do you approach patient education and ensure understanding?
Patient education is crucial for effective healthcare delivery. I approach it by first assessing the patient’s baseline knowledge and learning preferences. I use simple language, visual aids, and teach-back methods to ensure understanding. Additionally, I encourage questions and create a supportive environment where patients feel comfortable discussing their concerns. Follow-ups through phone calls or additional visits help reinforce the information provided.
63. Can you describe a time you had to lead a multidisciplinary team in patient care?
In a recent case, I led a multidisciplinary team for a patient with complex chronic conditions. I organized regular meetings to discuss the patient’s progress, coordinated between specialists, and ensured everyone was aligned with the treatment plan. I emphasized communication and collaboration, which helped streamline the care process and resulted in improved patient outcomes. This experience reinforced the importance of teamwork in delivering comprehensive care.
64. What strategies do you use to manage a high patient load effectively?
- Prioritization: I assess each patient’s urgency and complexity, prioritizing those who need immediate attention.
- Delegation: I utilize the skills of my team, delegating tasks appropriately to ensure efficient workflow.
- Time Management: I allocate specific time slots for patient visits and stick to them, while also allowing flexibility for emergencies.
These strategies help maintain high-quality care even during peak times, ensuring that all patients receive the attention they deserve.
65. How do you stay current with medical advancements and incorporate them into practice?
I stay current with medical advancements through continuous education, attending seminars, and subscribing to relevant journals. I also participate in online forums and professional networks where I can exchange knowledge with peers. When incorporating new practices, I evaluate the evidence, consider the patient population, and collaborate with colleagues to ensure that any changes improve patient outcomes while aligning with best practices.
How to Prepare for Your Physician Assistant Interview
Preparing for a Physician Assistant interview requires a strategic approach to showcase your clinical knowledge, interpersonal skills, and commitment to patient care. Here are essential tips to help you stand out and make a positive impression during your interview.
- Research the Institution: Understand the mission, values, and specialties of the institution you are applying to. Tailor your responses to align with their objectives and demonstrate your genuine interest in contributing to their team.
- Review Common Interview Questions: Familiarize yourself with frequently asked Physician Assistant interview questions, such as those related to clinical scenarios, teamwork, and patient management. Practice articulating your responses clearly and confidently.
- Prepare Your Personal Story: Be ready to discuss your journey to becoming a Physician Assistant. Highlight your relevant experiences, motivations, and how your background has prepared you for this role. This personal connection can resonate with interviewers.
- Highlight Clinical Experience: Be prepared to discuss your hands-on clinical experience, including rotations, internships, and any patient interactions. Use specific examples to showcase your skills in patient assessment, treatment planning, and collaboration with healthcare teams.
- Understand the PA Role: Be knowledgeable about the scope of practice, responsibilities, and challenges faced by Physician Assistants. This understanding will help you articulate how you can contribute effectively to the healthcare team and patient care.
- Prepare Questions for Interviewers: Have thoughtful questions ready to ask your interviewers about the role, team dynamics, and opportunities for professional development. This shows your interest in the position and helps you assess if it’s the right fit for you.
- Practice Professionalism: Dress appropriately, maintain good body language, and exhibit confidence throughout the interview. Being professional and courteous creates a positive impression and reflects your readiness to be a part of a healthcare team.
Common Physician Assistant Interview Mistakes to Avoid
Interviewing for a Physician Assistant position can be challenging. Understanding common mistakes can significantly improve your chances of success. Here are eight mistakes to avoid during your interview process.
- Inadequate Research: Failing to research the healthcare facility and its values can make you seem unprepared. Demonstrating knowledge about the organization’s mission and specialty areas shows genuine interest and commitment.
- Weak Communication Skills: Effective communication is crucial for PAs. Avoid rambling or providing vague answers. Practice clear and concise responses that highlight your experience and skills relevant to the position.
- Not Practicing Behavioral Questions: Many interviews include behavioral questions. Not preparing for these can hinder your ability to present real-life scenarios effectively. Use the STAR method (Situation, Task, Action, Result) to structure your responses.
- Ignoring the Team Dynamic: PAs work in teams with physicians and nurses. Neglecting to discuss your collaborative skills can raise concerns. Emphasize your ability to work effectively within a multidisciplinary team.
- Overlooking Questions for the Interviewer: Not asking questions can suggest a lack of interest. Prepare thoughtful questions about the role, team structure, and patient care philosophy to demonstrate your enthusiasm and critical thinking.
- Failure to Discuss Continuing Education: The medical field is constantly evolving. Not mentioning your commitment to ongoing education and staying current with medical guidelines may lead to doubts about your dedication to professional growth.
- Neglecting to Follow-Up: Failing to send a thank-you note after the interview can be a missed opportunity. A follow-up note expresses gratitude and reinforces your interest in the position, leaving a positive impression.
- Being Unprepared for Clinical Scenarios: You may be asked to solve clinical scenarios or answer technical questions. Not preparing for these can reflect poorly on your clinical judgment. Review common medical cases and practice articulating your thought process.
Key Takeaways for Physician Assistant Interview Success
- Prepare a strong resume using an AI resume builder to highlight your skills and experiences effectively. Tailor your resume to the specific requirements of the Physician Assistant position.
- Utilize professional resume templates to ensure a clean and organized presentation of your qualifications. A well-structured resume can make a significant impact on hiring managers.
- Showcase relevant experience by referring to resume examples that align with the Physician Assistant role. Use these as a guide to emphasize your clinical skills and patient care background.
- Craft personalized cover letters that reflect your passion for healthcare and commitment to patient welfare. A compelling cover letter can set you apart from other candidates.
- Engage in mock interview practice to build confidence and hone your communication skills. This preparation will help you articulate your thoughts clearly during the actual interview.
Frequently Asked Questions
1. How long does a typical Physician Assistant interview last?
A typical Physician Assistant interview usually lasts between 30 to 60 minutes. During this time, interviewers assess your clinical knowledge, communication skills, and ability to work in a team. The interview may include questions about your experience, case scenarios, and your understanding of the PA role. Be prepared for both technical and behavioral questions, and ensure you have questions ready for the interviewers to demonstrate your interest in the position.
2. What should I wear to a Physician Assistant interview?
For a Physician Assistant interview, it’s best to wear professional attire that reflects the seriousness of the role. A business suit, dress shirt, and dress shoes are ideal for both men and women. Ensure your clothes are clean, pressed, and fit well. Avoid overly casual clothing and excessive accessories. Dressing professionally demonstrates respect for the interviewers and the profession, helping you make a positive first impression.
3. How many rounds of interviews are typical for a Physician Assistant position?
Typically, the interview process for a Physician Assistant position may involve two to three rounds. The first round is often a screening interview, which may be conducted by a recruiter or HR personnel. Subsequent rounds usually involve direct interviews with hiring managers, physicians, or potential colleagues. Each round may focus on different aspects, such as clinical skills, teamwork, and cultural fit within the organization, so be prepared for varied questions.
4. Should I send a thank-you note after my Physician Assistant interview?
Yes, sending a thank-you note after your Physician Assistant interview is highly recommended. It shows appreciation for the interviewers’ time and reinforces your interest in the position. Aim to send a thoughtful note within 24 hours of your interview, either via email or handwritten. In your message, briefly reiterate your enthusiasm for the role and highlight any key points from the discussion that resonated with you, which can help you stand out among other candidates.